Drug utilization management criteria, such as Prior Authorizations (PAs), step therapy, and quantity limits, are designed to optimize patient outcomes and reduce waste, errors, unnecessary drug use, & costs. These programs are essential for controlling healthcare costs, influencing patient care decisions, and improving the quality of treatment. Collaboration between prescribers, payers, and pharmacists has become more emphasized to ensure patients receive timely access to drugs while maintaining cost-effectiveness and value. The future of utilization management involves a growing reliance on pharmacists in the PA process, the adoption of Electronic PA (ePA) to streamline approvals, and the development of best practices & national standards for electronic health information exchange.
The need for cost containment in healthcare is further emphasized by the fact that the U.S. spends a substantial portion of its GDP on healthcare, with prescription drugs being a major source of this expenditure. According to the U.S. Centers for Medicare & Medicaid Services (CMS), in 2025, the U.S. spent USD 4.9 trillion on healthcare services, and around USD 449.7 billion was spent on prescription drugs in 2023, which is a 11.4% increase from 2022. To manage these costs effectively, healthcare providers and payers are implementing various strategies, including UM, which involves the use of clinical guidelines, formularies, and other tools to ensure that patients receive the most appropriate & cost-effective treatments. This approach not only helps reduce healthcare costs but also improves patient outcomes by ensuring that patients receive the best possible care.
U.S. Drug Utilization Management Market Report Segmentation
This report forecasts revenue growth at the country level and provides an analysis of the latest industry trends and opportunities in each of the sub-segments from 2021 to 2033. For this study, the analyst has segmented the U.S. drug utilization management market report based on program type and end-use:Program Type Outlook (Revenue, USD Billion, 2021-2033)
End-use Outlook (Revenue, USD Billion, 2021-2033)
Why You Should Buy This Report
- Comprehensive Market Analysis: Gain detailed insights into the market across major regions and segments.
- Competitive Landscape: Explore the market presence of key players.
- Future Trends: Discover the pivotal trends and drivers shaping the future of the market.
- Actionable Recommendations: Utilize insights to uncover new revenue streams and guide strategic business decisions.
Report Deliverables
- Market intelligence to enable effective decision-making
- Market estimates and forecasts from 2018 to 2030
- Growth opportunities and trend analyses
- Segment and regional revenue forecasts for market assessment
- Competition strategy and market share analysis
- Product innovation listings for you to stay ahead of the curve
This product will be delivered within 1-3 business days.
Table of Contents
Companies Mentioned
The companies profiled in this U.S. Drug Utilization Management market report include:- Third Party Providers:
- Prime Therapeutics LLC
- MedicusRx
- EmblemHealth
- Optum, Inc.
- Point32Health, Inc.
- AssureCare LLC
- MindRx Group
- Agadia Systems, Inc
- Elevance Health (CarelonRx)
- ExlService Holdings, Inc.
- MRIoA
- S&C Technologies, Inc.
- In-House Providers
- Ultimate Health Plans
- Security Health Plan of Wisconsin, Inc.
- Blue Cross and Blue Shield Association
- Providence
- Simply Healthcare Plans, Inc
- Health Plan of San Mateo (HPSM)
- PerformRx
- Aetna, Inc. (CVS Health Corp.)
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 140 |
| Published | October 2025 |
| Forecast Period | 2024 - 2033 |
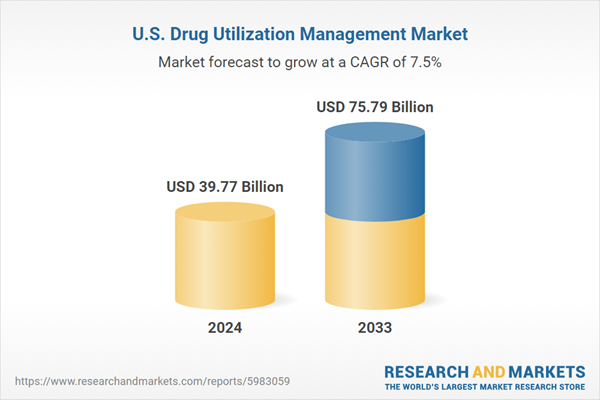
| Estimated Market Value ( USD | $ 39.77 Billion |
| Forecasted Market Value ( USD | $ 75.79 Billion |
| Compound Annual Growth Rate | 7.4% |
| Regions Covered | United States |
| No. of Companies Mentioned | 23 |