Global Healthcare Electronic Data Interchange (EDI) Market - Key Trends and Drivers Summarized
Why Is Healthcare Electronic Data Interchange (EDI) Becoming Essential for Streamlining Data Exchange, Improving Efficiency, and Reducing Costs in Healthcare?
Healthcare Electronic Data Interchange (EDI) has become essential for streamlining data exchange, improving efficiency, and reducing costs across the healthcare industry. But why is healthcare EDI so critical today? As healthcare organizations process vast amounts of information daily - ranging from patient records, insurance claims, to billing data - traditional methods of exchanging this information, such as paper forms or manual data entry, are inefficient, error-prone, and time-consuming. EDI provides a standardized, automated solution that enables the secure electronic exchange of healthcare-related information between providers, payers, and other stakeholders. By eliminating manual processes, healthcare EDI reduces errors, accelerates workflows, and enhances the accuracy of data.EDI is especially valuable in claims processing and reimbursement, where speed and accuracy are paramount. By automating the transmission of insurance claims, healthcare providers can receive payments more quickly, reduce claim rejections due to errors, and ensure that critical information is processed correctly. Moreover, healthcare EDI enhances communication between various entities within the healthcare ecosystem - such as hospitals, labs, pharmacies, and insurance companies - ensuring that vital information is transmitted seamlessly and securely. The result is improved operational efficiency, lower administrative costs, and better patient care.
How Are Technological Advancements and Innovations Improving the Accuracy, Security, and Scalability of Healthcare EDI?
Technological advancements are significantly improving the accuracy, security, and scalability of healthcare EDI, making it easier for healthcare organizations to exchange data in a faster, more reliable manner. One of the most impactful innovations is the integration of cloud-based EDI platforms. These cloud solutions allow healthcare providers and payers to access EDI systems from anywhere, offering greater flexibility and scalability. Cloud-based EDI systems eliminate the need for expensive on-premise infrastructure, reduce maintenance costs, and provide seamless updates to ensure compliance with the latest healthcare standards. Additionally, the cloud enables secure data storage and faster transmission of EDI transactions, improving the overall efficiency of healthcare data exchange.The adoption of advanced encryption technologies is another key advancement in healthcare EDI. Given the sensitive nature of healthcare information, securing EDI transactions is critical to maintaining patient confidentiality and complying with regulations like the Health Insurance Portability and Accountability Act (HIPAA). Encryption technologies protect healthcare data as it is transmitted between organizations, ensuring that only authorized users can access or alter the information. These encryption protocols, coupled with secure communication channels, prevent data breaches, mitigate the risks of cyberattacks, and ensure that healthcare organizations maintain compliance with strict data security regulations.
Artificial intelligence (AI) and machine learning (ML) are playing an increasingly important role in improving the accuracy of healthcare EDI. AI-powered EDI systems can automatically detect and correct errors in data entries, such as incorrect patient information, coding mistakes, or mismatches in insurance claim details. These technologies continuously learn from past transactions, becoming more accurate over time in identifying and resolving discrepancies. Machine learning algorithms also help EDI systems predict and prevent potential errors, allowing healthcare providers to submit cleaner, more accurate claims that are less likely to be rejected by insurance payers.
Blockchain technology is emerging as a powerful tool for enhancing the transparency and security of healthcare EDI. Blockchain's decentralized ledger ensures that every transaction or data exchange is recorded in a tamper-proof and auditable manner. In healthcare EDI, this means that patient records, insurance claims, and other sensitive data can be exchanged with a verified chain of custody, reducing the risk of fraud and ensuring data integrity. Blockchain also makes it easier for healthcare providers and payers to trace the source of any discrepancies or errors in data transactions, improving accountability and trust across the healthcare supply chain.
The use of robotic process automation (RPA) is further enhancing the efficiency of healthcare EDI by automating repetitive tasks such as data entry, validation, and claims processing. RPA bots can handle large volumes of EDI transactions, freeing up administrative staff to focus on higher-value tasks such as patient care and resolving complex claims issues. These bots can quickly process information from multiple sources, such as billing systems and EHR platforms, and ensure that the correct data is transmitted between parties, reducing processing times and improving overall efficiency.
Why Is Healthcare EDI Critical for Reducing Errors, Accelerating Claims Processing, and Ensuring Regulatory Compliance?
Healthcare EDI is critical for reducing errors, accelerating claims processing, and ensuring regulatory compliance because it provides a standardized and automated method for exchanging healthcare information, reducing the likelihood of manual data entry errors and ensuring accuracy. One of the primary reasons healthcare EDI is so valuable is its ability to minimize data entry mistakes, which are a common source of delays and rejections in claims processing. By automating data exchanges between healthcare providers, insurance companies, and other stakeholders, EDI eliminates the need for manual input, significantly reducing human errors and ensuring that patient information, billing details, and insurance codes are accurate and consistent.Accelerating claims processing is another significant benefit of healthcare EDI. Traditional claims processing methods, which rely on paper forms and manual verification, are time-consuming and prone to delays. EDI speeds up this process by enabling healthcare providers to submit claims electronically, reducing processing times from weeks to just days. This faster turnaround helps healthcare organizations maintain a steady cash flow, as claims are processed more quickly and reimbursements are received sooner. Additionally, automated error-checking tools built into EDI systems ensure that claims are clean and complete before submission, reducing the likelihood of denials and rework, which can further accelerate the reimbursement process.
Ensuring regulatory compliance is another key function of healthcare EDI. The healthcare industry is subject to a wide range of regulatory requirements, including HIPAA, which mandates the secure transmission of patient health information (PHI). EDI solutions are designed to comply with these regulations, providing encryption, secure data exchange protocols, and audit trails that allow healthcare organizations to track and verify every transaction. This level of compliance is critical for protecting patient data, avoiding regulatory fines, and ensuring that healthcare providers and payers adhere to legal and ethical standards for data security.
Healthcare EDI also plays a critical role in improving communication and coordination between different entities within the healthcare system. For example, when a patient is referred to a specialist, healthcare EDI can facilitate the secure exchange of medical records between the primary care provider and the specialist. This improves care coordination by ensuring that all parties have access to the same accurate and up-to-date information, reducing the risk of miscommunication or treatment delays. In addition, EDI helps streamline communications between healthcare providers and insurance companies, making it easier to verify patient eligibility, check the status of claims, and resolve any issues that arise during the billing and reimbursement process.
Another benefit of healthcare EDI is its ability to support population health management initiatives by providing healthcare organizations with timely and accurate data on patient demographics, treatment outcomes, and healthcare utilization. EDI systems enable healthcare providers to analyze trends in patient care, identify gaps in service delivery, and allocate resources more effectively. This can lead to improved patient outcomes and a more efficient healthcare system overall. Moreover, EDI helps healthcare organizations manage large volumes of data more efficiently, reducing the administrative burden on staff and enabling them to focus more on patient care and less on paperwork.
What Factors Are Driving the Growth of the Healthcare EDI Market?
Several key factors are driving the rapid growth of the healthcare EDI market, including the increasing adoption of electronic health records (EHR), the growing demand for cost-efficient healthcare solutions, the rise of value-based care models, and the need for improved data security and regulatory compliance. One of the primary drivers is the widespread adoption of EHR systems, which have digitized patient records and made it easier to share data between healthcare providers, payers, and other stakeholders. As more healthcare organizations implement EHR systems, the need for seamless data exchange solutions like EDI has grown. EDI ensures that patient information, billing codes, and insurance claims are transmitted accurately and efficiently between systems, reducing the risk of errors and delays.The growing demand for cost-efficient healthcare solutions is another major factor fueling the expansion of the healthcare EDI market. As healthcare costs continue to rise, providers are under pressure to find ways to reduce administrative expenses while improving operational efficiency. EDI helps healthcare organizations achieve these goals by automating many of the manual processes involved in data exchange, such as claims submission, billing, and patient eligibility verification. By reducing the time and effort required to process these transactions, EDI enables healthcare providers to lower their administrative costs and allocate resources more effectively.
The shift toward value-based care models is another significant driver of growth in the healthcare EDI market. Value-based care emphasizes improving patient outcomes while controlling costs, which requires healthcare organizations to closely monitor and analyze performance data. EDI plays a critical role in facilitating this data exchange by enabling healthcare providers to share patient information, treatment outcomes, and cost data with payers in a standardized format. This data is essential for tracking key performance indicators (KPIs) such as patient satisfaction, readmission rates, and treatment effectiveness, all of which are central to value-based care initiatives.
The increasing need for improved data security and regulatory compliance is also contributing to the growth of the healthcare EDI market. With the rise of cyberattacks and data breaches, healthcare organizations are under more pressure than ever to protect sensitive patient information. EDI solutions provide robust security features, including encryption and secure communication protocols, to ensure that data is transmitted safely between parties. In addition, EDI helps healthcare organizations comply with data privacy regulations such as HIPAA, which require strict safeguards for the handling and transmission of protected health information (PHI). As regulatory requirements continue to evolve, healthcare providers are investing in EDI solutions to ensure compliance and avoid costly fines or penalties.
Another important factor driving the market's growth is the increasing complexity of healthcare billing and coding systems. With a growing number of insurance plans, payment models, and treatment codes, healthcare providers must navigate a complex landscape when submitting claims and verifying patient eligibility. EDI simplifies this process by automating the exchange of billing codes, insurance information, and payment details, ensuring that all parties have access to accurate and up-to-date information. This level of automation is particularly valuable as healthcare organizations deal with an increasing volume of transactions and need to minimize errors and delays.
In conclusion, the growth of the healthcare EDI market is driven by the increasing adoption of EHRs, the demand for cost-efficient healthcare solutions, the shift toward value-based care models, and the need for improved data security and regulatory compliance. As healthcare organizations continue to digitize their operations and seek ways to reduce administrative costs, healthcare EDI will play an increasingly important role in streamlining data exchange, enhancing operational efficiency, and improving patient outcomes.
Report Scope
The report analyzes the Healthcare Electronic Data Interchange (EDI) market, presented in terms of market value (USD). The analysis covers the key segments and geographic regions outlined below.- Segments: Component (Services, Solutions); Deployment (Web & Cloud EDI, Mobile EDI, EDI VAN (Value Added Network), Direct (Point-to-Point) EDI); End-Use (Healthcare Payers, Healthcare Providers, Pharmaceutical & Medical Device Companies, Other End-Uses).
- Geographic Regions/Countries: World; United States; Canada; Japan; China; Europe (France; Germany; Italy; United Kingdom; and Rest of Europe); Asia-Pacific; Rest of World.
Key Insights:
- Market Growth: Understand the significant growth trajectory of the Services Component segment, which is expected to reach US$5.7 Billion by 2030 with a CAGR of 7.6%. The Solutions Component segment is also set to grow at 10.9% CAGR over the analysis period.
- Regional Analysis: Gain insights into the U.S. market, valued at $1.6 Billion in 2024, and China, forecasted to grow at an impressive 12.9% CAGR to reach $2.6 Billion by 2030. Discover growth trends in other key regions, including Japan, Canada, Germany, and the Asia-Pacific.
Why You Should Buy This Report:
- Detailed Market Analysis: Access a thorough analysis of the Global Healthcare Electronic Data Interchange (EDI) Market, covering all major geographic regions and market segments.
- Competitive Insights: Get an overview of the competitive landscape, including the market presence of major players across different geographies.
- Future Trends and Drivers: Understand the key trends and drivers shaping the future of the Global Healthcare Electronic Data Interchange (EDI) Market.
- Actionable Insights: Benefit from actionable insights that can help you identify new revenue opportunities and make strategic business decisions.
Key Questions Answered:
- How is the Global Healthcare Electronic Data Interchange (EDI) Market expected to evolve by 2030?
- What are the main drivers and restraints affecting the market?
- Which market segments will grow the most over the forecast period?
- How will market shares for different regions and segments change by 2030?
- Who are the leading players in the market, and what are their prospects?
Report Features:
- Comprehensive Market Data: Independent analysis of annual sales and market forecasts in US$ Million from 2024 to 2030.
- In-Depth Regional Analysis: Detailed insights into key markets, including the U.S., China, Japan, Canada, Europe, Asia-Pacific, Latin America, Middle East, and Africa.
- Company Profiles: Coverage of players such as Allscripts Healthcare Solutions, Inc., Cerner Corporation, Cognizant Technology Solutions Corporation, Dell Technologies, Experian PLC and more.
- Complimentary Updates: Receive free report updates for one year to keep you informed of the latest market developments.
Some of the 28 companies featured in this Healthcare Electronic Data Interchange (EDI) market report include:
- Allscripts Healthcare Solutions, Inc.
- Cerner Corporation
- Cognizant Technology Solutions Corporation
- Dell Technologies
- Experian PLC
- GE Healthcare
- McKesson Corporation
- Optum, Inc.
- Quality Systems, Inc.
- SSI Group
- Synnex Corporation
This edition integrates the latest global trade and economic shifts into comprehensive market analysis. Key updates include:
- Tariff and Trade Impact: Insights into global tariff negotiations across 180+ countries, with analysis of supply chain turbulence, sourcing disruptions, and geographic realignment. Special focus on 2025 as a pivotal year for trade tensions, including updated perspectives on the Trump-era tariffs.
- Adjusted Forecasts and Analytics: Revised global and regional market forecasts through 2030, incorporating tariff effects, economic uncertainty, and structural changes in globalization. Includes historical analysis from 2015 to 2023.
- Strategic Market Dynamics: Evaluation of revised market prospects, regional outlooks, and key economic indicators such as population and urbanization trends.
- Innovation & Technology Trends: Latest developments in product and process innovation, emerging technologies, and key industry drivers shaping the competitive landscape.
- Competitive Intelligence: Updated global market share estimates for 2025, competitive positioning of major players (Strong/Active/Niche/Trivial), and refined focus on leading global brands and core players.
- Expert Insight & Commentary: Strategic analysis from economists, trade experts, and domain specialists to contextualize market shifts and identify emerging opportunities.
Table of Contents
Companies Mentioned (Partial List)
A selection of companies mentioned in this report includes, but is not limited to:
- Allscripts Healthcare Solutions, Inc.
- Cerner Corporation
- Cognizant Technology Solutions Corporation
- Dell Technologies
- Experian PLC
- GE Healthcare
- McKesson Corporation
- Optum, Inc.
- Quality Systems, Inc.
- SSI Group
- Synnex Corporation
Table Information
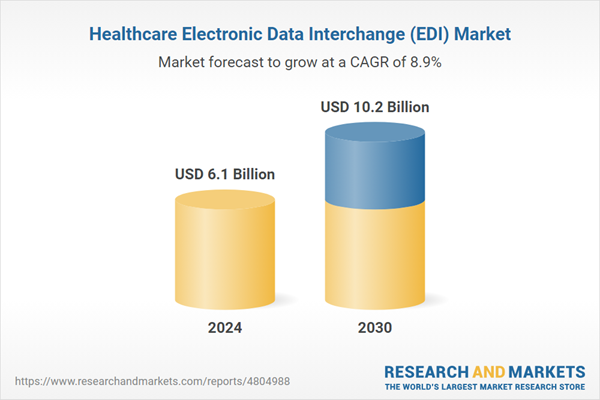
| Report Attribute | Details |
|---|---|
| No. of Pages | 237 |
| Published | January 2026 |
| Forecast Period | 2024 - 2030 |
| Estimated Market Value ( USD | $ 6.1 Billion |
| Forecasted Market Value ( USD | $ 10.2 Billion |
| Compound Annual Growth Rate | 8.9% |
| Regions Covered | Global |