Global Human Liver Models Market - Key Trends and Drivers Summarized
Are Human Liver Models the Future of Drug Development, Disease Research, and Toxicology Testing?
Human liver models have emerged as a vital tool in biomedical research, but why are they so essential for advancing drug development, disease research, and toxicology testing? Human liver models refer to in vitro systems, such as liver-on-a-chip, 3D bioprinted liver tissues, organoids, and cell culture models, that mimic the structure and function of the human liver. These models allow scientists to study liver function, drug metabolism, liver diseases, and toxicological effects without relying on animal models or human clinical trials.The importance of human liver models lies in their ability to provide more accurate and human-relevant data for studying liver function and disease mechanisms. Traditional animal models often fail to accurately represent human biology, leading to issues in drug development and toxicology. Human liver models offer a powerful alternative, allowing for more precise testing of drug efficacy, liver toxicity, and metabolic processes. As personalized medicine, biotechnology, and pharmaceutical industries expand, human liver models are critical for improving the accuracy of drug discovery, reducing reliance on animal testing, and better understanding liver diseases.
How Has Technology Advanced Human Liver Models?
Technological advancements have significantly improved the development and functionality of human liver models, making them more accurate and versatile for various biomedical applications. One of the most significant breakthroughs is the advent of liver-on-a-chip technology, where miniaturized liver systems are created using microfluidic devices that mimic the dynamic environment of the liver. These chips contain live human liver cells and microchannels that replicate blood flow, providing a highly realistic model of liver physiology. This technology allows researchers to study how the liver metabolizes drugs and toxins in a controlled environment, delivering more predictive data for drug development.3D bioprinting is another transformative technology advancing human liver models. Using bioinks made from liver cells and other biological materials, scientists can now print liver tissues with the same complex structure as a human liver. These 3D bioprinted liver tissues provide a better representation of the liver's microarchitecture, improving the accuracy of in vitro studies. The ability to bioprint liver tissues also opens the door for creating patient-specific liver models, which can be used for personalized drug testing and disease modeling, helping doctors predict how an individual's liver will respond to specific treatments.
Organoid technology has also revolutionized human liver models. Liver organoids are miniature, self-organizing 3D structures derived from stem cells that replicate many of the liver's key functions. These organoids provide a valuable platform for studying liver regeneration, disease progression, and drug metabolism. They are especially useful for modeling liver diseases, such as hepatitis or non-alcoholic fatty liver disease (NAFLD), and testing the effects of new drugs in a more human-like system. Organoids also have potential in regenerative medicine, as they could one day be used to repair or replace damaged liver tissues.
Improvements in stem cell technologies, particularly the use of induced pluripotent stem cells (iPSCs), have enhanced the development of personalized liver models. iPSCs can be derived from a patient's own cells and then differentiated into liver cells (hepatocytes), offering the ability to create liver models that are genetically identical to the patient. These personalized liver models allow for drug screening and toxicity testing that reflects individual patient responses, making drug development more tailored and precise.
Another advancement is the integration of artificial intelligence (AI) and machine learning in liver model research. AI algorithms can analyze large datasets from liver models, identifying patterns in drug metabolism or disease progression that may not be obvious to researchers. AI-powered tools can also optimize the design of liver-on-a-chip systems or predict the outcomes of drug treatments based on the model's response, further accelerating the research process.
Why Are Human Liver Models Critical for Drug Development and Disease Research?
Human liver models are critical for drug development, disease research, and toxicology testing because they provide a more accurate and human-relevant platform for understanding how drugs and diseases interact with the liver. The liver plays a central role in metabolizing drugs and toxins, making it a key focus in drug safety testing. Traditional animal models often fail to predict how a human liver will respond to new drugs due to significant differences in metabolism between species. Human liver models, on the other hand, replicate the cellular and physiological characteristics of human liver function, providing more accurate data on drug metabolism, efficacy, and potential toxicity.One of the most important applications of human liver models is in preclinical drug testing. Before a new drug can enter clinical trials, it must be tested for its safety and effectiveness, particularly in relation to liver function. Human liver models allow researchers to assess how a drug will be metabolized and whether it has any toxic effects on the liver, helping to identify potential issues early in the development process. This reduces the likelihood of drugs failing in late-stage clinical trials due to unforeseen liver toxicity, saving time, resources, and costs for pharmaceutical companies.
Human liver models are also invaluable for studying liver diseases, such as hepatitis, cirrhosis, and liver cancer. By using liver-on-a-chip systems, 3D bioprinted tissues, or organoids, researchers can recreate the conditions of liver diseases in vitro, enabling them to study disease mechanisms, progression, and potential treatments. These models provide insights into how liver diseases affect liver function at the cellular level, helping to develop more effective therapies. For instance, liver models can be used to test antiviral drugs for hepatitis or investigate the efficacy of new treatments for liver cancer.
Toxicology testing is another critical area where human liver models play a crucial role. Many chemicals and environmental toxins can have harmful effects on the liver, leading to conditions such as liver damage or failure. Human liver models provide a safer, more ethical way to test the toxicity of various substances compared to traditional animal testing. These models allow for high-throughput screening of chemicals, enabling researchers to quickly and efficiently determine which compounds are safe and which pose risks to liver health.
Personalized medicine is also benefiting from the use of human liver models. By creating liver models derived from a patient's own cells, healthcare providers can test how a patient's liver will respond to specific drugs before administering treatment. This is particularly important for patients with liver diseases or those undergoing treatments that are known to impact liver function, such as chemotherapy. Personalized liver models help to minimize the risk of adverse drug reactions and ensure that patients receive the most effective treatments for their unique biological makeup.
In addition, human liver models are being used in regenerative medicine to explore potential therapies for liver repair and regeneration. For example, liver organoids and bioprinted tissues could one day be used to repair damaged liver tissue in patients with liver disease, reducing the need for liver transplants. These models provide a platform for testing new cell-based therapies and understanding how liver cells regenerate, offering hope for patients with chronic liver conditions.
What Factors Are Driving the Growth of the Human Liver Model Market?
Several factors are driving the growth of the human liver model market, including the increasing demand for more accurate drug testing, advancements in 3D bioprinting and organoid technologies, and the growing focus on personalized medicine. One of the primary drivers is the need for more predictive models in drug development. As the cost of drug development continues to rise, pharmaceutical companies are looking for ways to reduce the failure rate of new drugs in clinical trials. Human liver models offer a more reliable method for predicting how drugs will interact with the human liver, leading to better preclinical testing and fewer costly trial failures due to liver toxicity.The push for alternatives to animal testing is another significant factor driving market growth. Regulatory bodies, such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), are encouraging the use of in vitro models as alternatives to animal testing. Human liver models provide a more ethical and human-relevant option for toxicity testing, aligning with global efforts to reduce animal use in research. This shift toward more ethical testing methods is expected to drive further adoption of liver models in toxicology testing.
Advancements in 3D bioprinting and organoid technologies are also contributing to the growth of the human liver model market. These technologies allow researchers to create more sophisticated and functional liver models that closely replicate the complexity of the human liver. The ability to print 3D liver tissues or grow liver organoids from stem cells opens up new possibilities for studying liver diseases, drug metabolism, and liver regeneration. As these technologies continue to evolve, they are expected to become more widely used in research and drug development.
The rise of personalized medicine is another key driver. As healthcare moves toward more individualized treatment plans, there is a growing need for models that can predict how specific patients will respond to drugs. Human liver models created from patient-derived cells enable researchers to test the effects of drugs on a patient's liver function, providing more tailored and effective treatment options. This trend is particularly strong in fields such as oncology and liver disease, where patient-specific liver models can be used to optimize treatment plans and reduce the risk of adverse drug reactions.
The increasing prevalence of liver diseases, such as non-alcoholic fatty liver disease (NAFLD), cirrhosis, and liver cancer, is also driving demand for better liver models. As the global burden of liver disease rises, there is a growing need for accurate models that can help researchers develop new therapies and better understand disease mechanisms. Human liver models provide a more relevant and precise tool for studying liver diseases, accelerating the development of treatments that can improve patient outcomes.
With advancements in bioprinting, organoid technologies, and personalized medicine, the human liver model market is poised for significant growth. As the demand for more accurate, ethical, and human-relevant testing methods increases, human liver models will remain a key tool for advancing drug development, improving disease research, and reducing reliance on animal testing in toxicology studies.
Report Scope
The report analyzes the Human Liver Models market, presented in terms of market value (USD). The analysis covers the key segments and geographic regions outlined below.- Segments: Type (Liver Organoids, Liver-On-A-Chip, 3D Bioprinting, 2D Models, Other Types); Application (Drug Discovery, Educational, Other Applications).
- Geographic Regions/Countries: World; United States; Canada; Japan; China; Europe (France; Germany; Italy; United Kingdom; Spain; Russia; and Rest of Europe); Asia-Pacific (Australia; India; South Korea; and Rest of Asia-Pacific); Latin America (Argentina; Brazil; Mexico; and Rest of Latin America); Middle East (Iran; Israel; Saudi Arabia; United Arab Emirates; and Rest of Middle East); and Africa.
Key Insights:
- Market Growth: Understand the significant growth trajectory of the Drug Discovery Application segment, which is expected to reach US$225.8 Million by 2030 with a CAGR of 9.1%. The Educational Application segment is also set to grow at 10.4% CAGR over the analysis period.
- Regional Analysis: Gain insights into the U.S. market, valued at $74.4 Million in 2024, and China, forecasted to grow at an impressive 13.2% CAGR to reach $104.6 Million by 2030. Discover growth trends in other key regions, including Japan, Canada, Germany, and the Asia-Pacific.
Why You Should Buy This Report:
- Detailed Market Analysis: Access a thorough analysis of the Global Human Liver Models Market, covering all major geographic regions and market segments.
- Competitive Insights: Get an overview of the competitive landscape, including the market presence of major players across different geographies.
- Future Trends and Drivers: Understand the key trends and drivers shaping the future of the Global Human Liver Models Market.
- Actionable Insights: Benefit from actionable insights that can help you identify new revenue opportunities and make strategic business decisions.
Key Questions Answered:
- How is the Global Human Liver Models Market expected to evolve by 2030?
- What are the main drivers and restraints affecting the market?
- Which market segments will grow the most over the forecast period?
- How will market shares for different regions and segments change by 2030?
- Who are the leading players in the market, and what are their prospects?
Report Features:
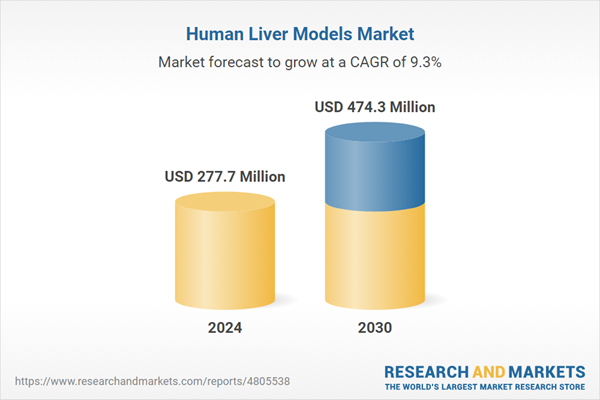
- Comprehensive Market Data: Independent analysis of annual sales and market forecasts in US$ Million from 2024 to 2030.
- In-Depth Regional Analysis: Detailed insights into key markets, including the U.S., China, Japan, Canada, Europe, Asia-Pacific, Latin America, Middle East, and Africa.
- Company Profiles: Coverage of players such as BioIVT, LLC., Charles River Laboratories International, Inc., CN Bio Innovations Ltd., Crown Bioscience, Inc., Cyfuse Biomedical K.K. and more.
- Complimentary Updates: Receive free report updates for one year to keep you informed of the latest market developments.
Some of the 42 companies featured in this Human Liver Models market report include:
- BioIVT, LLC.
- Charles River Laboratories International, Inc.
- CN Bio Innovations Ltd.
- Crown Bioscience, Inc.
- Cyfuse Biomedical K.K.
- Emulate, Inc.
- Mimetas
- Organovo Holdings, Inc.
- Taconic Biosciences, Inc.
- Yecuris
This edition integrates the latest global trade and economic shifts into comprehensive market analysis. Key updates include:
- Tariff and Trade Impact: Insights into global tariff negotiations across 180+ countries, with analysis of supply chain turbulence, sourcing disruptions, and geographic realignment. Special focus on 2025 as a pivotal year for trade tensions, including updated perspectives on the Trump-era tariffs.
- Adjusted Forecasts and Analytics: Revised global and regional market forecasts through 2030, incorporating tariff effects, economic uncertainty, and structural changes in globalization. Includes historical analysis from 2015 to 2023.
- Strategic Market Dynamics: Evaluation of revised market prospects, regional outlooks, and key economic indicators such as population and urbanization trends.
- Innovation & Technology Trends: Latest developments in product and process innovation, emerging technologies, and key industry drivers shaping the competitive landscape.
- Competitive Intelligence: Updated global market share estimates for 2025, competitive positioning of major players (Strong/Active/Niche/Trivial), and refined focus on leading global brands and core players.
- Expert Insight & Commentary: Strategic analysis from economists, trade experts, and domain specialists to contextualize market shifts and identify emerging opportunities.
Table of Contents
Companies Mentioned (Partial List)
A selection of companies mentioned in this report includes, but is not limited to:
- BioIVT, LLC.
- Charles River Laboratories International, Inc.
- CN Bio Innovations Ltd.
- Crown Bioscience, Inc.
- Cyfuse Biomedical K.K.
- Emulate, Inc.
- Mimetas
- Organovo Holdings, Inc.
- Taconic Biosciences, Inc.
- Yecuris
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 194 |
| Published | January 2026 |
| Forecast Period | 2024 - 2030 |
| Estimated Market Value ( USD | $ 277.7 Million |
| Forecasted Market Value ( USD | $ 474.2 Million |
| Compound Annual Growth Rate | 9.3% |
| Regions Covered | Global |