Global Humanized Mouse and Rat Model Market - Key Trends and Drivers Summarized
Are Humanized Mouse and Rat Models the Key to Breakthroughs in Biomedical Research and Precision Medicine?
Humanized mouse and rat models have revolutionized preclinical research, but why are they so essential for advancing drug development, immunology studies, and precision medicine? Humanized models refer to laboratory mice or rats that have been genetically modified or engrafted with human cells, tissues, or genes, enabling them to mimic human biological systems more closely. These models provide researchers with a powerful tool for studying human diseases, immune responses, cancer biology, and evaluating the safety and efficacy of new treatments before they proceed to clinical trials.The significance of humanized mouse and rat models lies in their ability to simulate human-specific responses that cannot be observed in conventional animal models. By using humanized models, researchers can study human immune function, infection mechanisms, and cancer progression with greater accuracy, bridging the gap between animal studies and human clinical trials. This improves the likelihood that experimental therapies and vaccines will succeed in humans. As precision medicine and immunotherapy continue to gain prominence, humanized models are playing a crucial role in advancing personalized healthcare and accelerating the development of life-saving treatments.
How Has Technology Advanced Humanized Mouse and Rat Models?
Technological advancements have significantly improved the development, functionality, and application of humanized mouse and rat models, making them more versatile and representative of human biology. One of the most important advancements is the ability to engraft human immune cells or tissues into immunodeficient mice. These mice lack functional immune systems, allowing human cells to survive and proliferate. Humanized immune system (HIS) mice are often used to study human immune responses to infections, autoimmune diseases, and cancer. For example, researchers can observe how human immune cells react to viral infections like HIV or COVID-19, gaining critical insights into the pathogenesis of these diseases and identifying potential therapeutic targets.The use of gene editing technologies, such as CRISPR-Cas9, has further advanced the development of humanized mouse and rat models. With CRISPR, researchers can precisely insert human genes into the genomes of mice or rats, creating models that express human proteins or receptors. This has been particularly useful in cancer research, where scientists can create humanized models that express human cancer-driving mutations or tumor suppressor genes. These models allow for the testing of targeted therapies, such as monoclonal antibodies or small-molecule inhibitors, in a system that closely mirrors human cancer biology.
Another major breakthrough is the development of humanized liver models. In these models, mice are engrafted with human hepatocytes (liver cells), making them ideal for studying human-specific drug metabolism, liver diseases, and toxicology. Humanized liver mice are invaluable for assessing how new drugs are metabolized in the human liver, helping to predict potential side effects or toxicities that might not be detected in traditional animal models. These models are also used to study hepatitis infections, offering a better understanding of how viral infections affect human liver function and aiding in the development of antiviral treatments.
Advances in human stem cell research have also contributed to the improvement of humanized models. Human pluripotent stem cells (hPSCs) can be differentiated into various human cell types, including immune cells, neurons, and pancreatic cells, which can then be engrafted into mice. These models are used to study human-specific biological processes, such as neurodegeneration in diseases like Alzheimer's or Parkinson's, diabetes, or even cardiovascular diseases. For example, humanized models with human neurons or glial cells enable researchers to investigate how these cells behave in a living organism, providing critical insights into neurological diseases and potential treatments.
The development of 'multi-tissue' humanized models is another significant advancement. These models are engrafted with several types of human tissues or organs, creating a more complete human biological environment. Multi-tissue humanized models allow researchers to study complex diseases, such as cancer metastasis, where interactions between different tissues (e.g., tumors and immune cells) are key to disease progression. This is particularly important for studying therapies that target multiple organs or systems, such as immunotherapies for cancer or treatments for autoimmune disorders.
Improved animal husbandry and breeding techniques have made it possible to produce humanized models more consistently and at scale. These techniques have streamlined the process of creating humanized mice and rats, ensuring that researchers have access to high-quality, reproducible models for their studies. In addition, advances in cryopreservation and transplantation techniques have made it easier to engraft human cells or tissues into animals, improving the overall success rate of creating viable humanized models.
Why Are Humanized Mouse and Rat Models Critical for Drug Development and Precision Medicine?
Humanized mouse and rat models are critical for drug development and precision medicine because they provide a more accurate representation of human biology, allowing for better predictions of how drugs will behave in humans. Traditional animal models, while useful, often fail to mimic human-specific responses to drugs, diseases, and therapies. Humanized models bridge this gap by incorporating human cells, genes, or tissues into animal systems, enabling researchers to study human disease mechanisms and drug effects in a more relevant context.In drug development, humanized models are particularly important for preclinical testing of new therapies. Before a drug can be tested in human clinical trials, it must undergo extensive testing in animal models to ensure its safety and efficacy. Humanized models allow researchers to observe how human cells or tissues react to potential therapies, reducing the risk of unexpected side effects or failures in human trials. For example, in oncology, humanized models can be used to test how human tumors respond to chemotherapy, targeted therapies, or immunotherapies like checkpoint inhibitors. By providing a more realistic model of how human cancer cells behave, these studies can help identify which therapies are most likely to be effective in clinical settings.
Humanized immune system (HIS) mice are also invaluable in immunotherapy research. Immunotherapies, such as CAR T-cell therapy or immune checkpoint inhibitors, rely on the patient's immune system to attack cancer cells. Testing these therapies in traditional animal models is challenging because mouse immune systems differ significantly from human immune systems. Humanized immune models, however, allow researchers to test immunotherapies on human immune cells in vivo, providing critical insights into how these therapies will perform in patients. This is particularly important for precision medicine, where treatments are tailored to individual patients based on their unique genetic and immunological profiles.
In addition to cancer research, humanized models are essential for studying infectious diseases. HIS mice are commonly used to investigate how human immune cells respond to infections like HIV, hepatitis, or COVID-19. By providing a model that mimics human immune responses, these studies help identify new therapeutic targets and test vaccines or antiviral drugs in a more accurate setting. For example, humanized mice were used in the development and testing of antiviral treatments and vaccines for COVID-19, playing a crucial role in understanding the virus's impact on human cells and immune responses.
Humanized liver models are particularly important for drug metabolism and toxicology studies. The human liver plays a central role in metabolizing drugs, and animal models often do not metabolize drugs in the same way as humans. Humanized liver mice allow researchers to study how new drugs are processed in the human liver, helping to identify potential toxicities or adverse effects before they are tested in human clinical trials. This reduces the likelihood of drug failures in late-stage trials, saving time and resources for pharmaceutical companies.
Humanized models are also key to advancing personalized and precision medicine. In precision medicine, treatments are tailored to an individual's specific genetic makeup, environment, and lifestyle. Humanized models, particularly those engrafted with patient-specific cells or tissues, enable researchers to test how an individual's unique biology responds to specific treatments. This approach is especially valuable in oncology, where therapies like targeted treatments or immunotherapies are designed based on a patient's tumor genetics or immune profile. By using humanized models to test these personalized therapies in preclinical studies, researchers can optimize treatments for individual patients and improve clinical outcomes.
What Factors Are Driving the Growth of the Humanized Mouse and Rat Model Market?
Several factors are driving the rapid growth of the humanized mouse and rat model market, including the increasing demand for more accurate preclinical models in drug development, advancements in gene editing technologies, and the rise of personalized medicine. One of the primary drivers is the need for more human-relevant models in drug discovery and development. Traditional animal models often fail to predict human responses accurately, leading to high failure rates in clinical trials. Humanized models offer a more reliable platform for testing the efficacy and safety of new drugs, reducing the likelihood of late-stage failures and improving the overall success rate of drug development programs.The rise of immunotherapies and targeted cancer treatments is another significant driver of the market. As immunotherapies become more widely used in treating cancer and other diseases, there is a growing need for models that can accurately replicate human immune responses. Humanized immune system (HIS) mice provide a crucial tool for testing these therapies, helping researchers optimize treatments and understand their mechanisms of action in a human-like immune environment. This is especially important as more pharmaceutical companies focus on developing personalized cancer treatments based on a patient's specific genetic or immunological profile.
Advancements in gene editing technologies, such as CRISPR-Cas9, have made it easier to create genetically modified humanized models. With CRISPR, researchers can precisely insert human genes into mouse or rat genomes, enabling the creation of highly specific models for studying diseases like cancer, Alzheimer's, and autoimmune disorders. These advancements have significantly increased the versatility and applicability of humanized models, making them an essential tool for researchers in a wide range of biomedical fields.
The growing interest in precision medicine is also driving demand for humanized models. Precision medicine aims to tailor treatments based on individual genetic and biological factors, and humanized models allow researchers to test therapies in a way that reflects human variability. By using humanized models engrafted with patient-specific cells or tissues, researchers can study how a particular patient's biology will respond to different treatments, improving the chances of successful outcomes in clinical settings.
The increasing prevalence of infectious diseases, particularly viral infections like HIV, hepatitis, and more recently, COVID-19, is further driving the growth of the humanized model market. These models are used to study how human immune cells respond to viral infections and to test potential vaccines or antiviral drugs. During the COVID-19 pandemic, humanized models played a critical role in understanding the virus's effects on human cells and testing vaccine candidates. As the global focus on infectious disease research continues to grow, humanized models will remain essential for developing effective treatments and vaccines.
Regulatory support and government initiatives are also contributing to market growth. Regulatory agencies, such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), are increasingly recognizing the value of humanized models in preclinical studies, particularly for testing biologics, immunotherapies, and personalized treatments. This regulatory support is encouraging pharmaceutical companies and research institutions to invest in humanized model development, further expanding the market.
With advancements in gene editing, the rise of immunotherapies, and the growing demand for precision medicine, the humanized mouse and rat model market is poised for significant growth. As researchers continue to seek more human-relevant models for drug development, disease research, and personalized healthcare, humanized models will remain a crucial tool for bridging the gap between preclinical studies and successful human treatments.
Report Scope
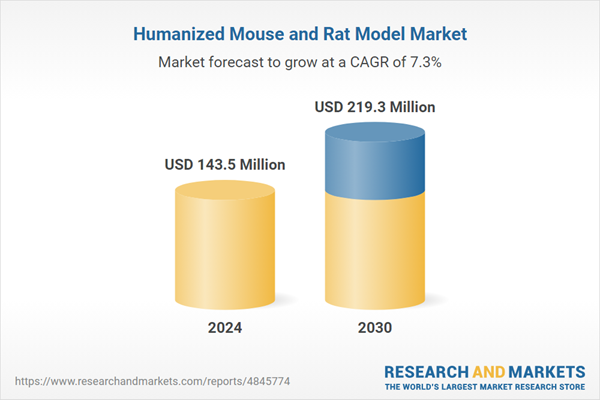
The report analyzes the Humanized Mouse and Rat Model market, presented in terms of market value (USD). The analysis covers the key segments and geographic regions outlined below.- Segments: Type (Humanized Mouse Models, Humanized Rat Models); Application (Oncology, Immunology & Infectious Diseases, Neuroscience, Hematopoesis, Other Applications); End-Use (Academic & Research Institutions, Pharma & Biotech Companies, Contract Research Organizations (CROs)).
- Geographic Regions/Countries: World; United States; Canada; Japan; China; Europe (France; Germany; Italy; United Kingdom; Spain; Russia; and Rest of Europe); Asia-Pacific (Australia; India; South Korea; and Rest of Asia-Pacific); Latin America (Argentina; Brazil; Mexico; and Rest of Latin America); Middle East (Iran; Israel; Saudi Arabia; United Arab Emirates; and Rest of Middle East); and Africa.
Key Insights:
- Market Growth: Understand the significant growth trajectory of the Oncology Application segment, which is expected to reach US$74.5 Million by 2030 with a CAGR of 7.9%. The Immunology & Infectious Diseases Application segment is also set to grow at 6.9% CAGR over the analysis period.
- Regional Analysis: Gain insights into the U.S. market, valued at $38.5 Million in 2024, and China, forecasted to grow at an impressive 10.8% CAGR to reach $47.3 Million by 2030. Discover growth trends in other key regions, including Japan, Canada, Germany, and the Asia-Pacific.
Why You Should Buy This Report:
- Detailed Market Analysis: Access a thorough analysis of the Global Humanized Mouse and Rat Model Market, covering all major geographic regions and market segments.
- Competitive Insights: Get an overview of the competitive landscape, including the market presence of major players across different geographies.
- Future Trends and Drivers: Understand the key trends and drivers shaping the future of the Global Humanized Mouse and Rat Model Market.
- Actionable Insights: Benefit from actionable insights that can help you identify new revenue opportunities and make strategic business decisions.
Key Questions Answered:
- How is the Global Humanized Mouse and Rat Model Market expected to evolve by 2030?
- What are the main drivers and restraints affecting the market?
- Which market segments will grow the most over the forecast period?
- How will market shares for different regions and segments change by 2030?
- Who are the leading players in the market, and what are their prospects?
Report Features:
- Comprehensive Market Data: Independent analysis of annual sales and market forecasts in US$ Million from 2024 to 2030.
- In-Depth Regional Analysis: Detailed insights into key markets, including the U.S., China, Japan, Canada, Europe, Asia-Pacific, Latin America, Middle East, and Africa.
- Company Profiles: Coverage of players such as Axenis S.A.S., Charles River Laboratories International, Inc., Crown Bioscience, Inc., Genoway S.A., Harbour Antibodies BV and more.
- Complimentary Updates: Receive free report updates for one year to keep you informed of the latest market developments.
Some of the 44 companies featured in this Humanized Mouse and Rat Model market report include:
- Axenis S.A.S.
- Charles River Laboratories International, Inc.
- Crown Bioscience, Inc.
- Genoway S.A.
- Harbour Antibodies BV
- Hera BioLabs
- inGenious Targeting Laboratory, Inc.
- Taconic Biosciences, Inc.
- The Jackson Laboratory
- Trans Genic, Inc.
This edition integrates the latest global trade and economic shifts into comprehensive market analysis. Key updates include:
- Tariff and Trade Impact: Insights into global tariff negotiations across 180+ countries, with analysis of supply chain turbulence, sourcing disruptions, and geographic realignment. Special focus on 2025 as a pivotal year for trade tensions, including updated perspectives on the Trump-era tariffs.
- Adjusted Forecasts and Analytics: Revised global and regional market forecasts through 2030, incorporating tariff effects, economic uncertainty, and structural changes in globalization. Includes historical analysis from 2015 to 2023.
- Strategic Market Dynamics: Evaluation of revised market prospects, regional outlooks, and key economic indicators such as population and urbanization trends.
- Innovation & Technology Trends: Latest developments in product and process innovation, emerging technologies, and key industry drivers shaping the competitive landscape.
- Competitive Intelligence: Updated global market share estimates for 2025, competitive positioning of major players (Strong/Active/Niche/Trivial), and refined focus on leading global brands and core players.
- Expert Insight & Commentary: Strategic analysis from economists, trade experts, and domain specialists to contextualize market shifts and identify emerging opportunities.
Table of Contents
Companies Mentioned (Partial List)
A selection of companies mentioned in this report includes, but is not limited to:
- Axenis S.A.S.
- Charles River Laboratories International, Inc.
- Crown Bioscience, Inc.
- Genoway S.A.
- Harbour Antibodies BV
- Hera BioLabs
- inGenious Targeting Laboratory, Inc.
- Taconic Biosciences, Inc.
- The Jackson Laboratory
- Trans Genic, Inc.
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 193 |
| Published | January 2026 |
| Forecast Period | 2024 - 2030 |
| Estimated Market Value ( USD | $ 143.5 Million |
| Forecasted Market Value ( USD | $ 219.4 Million |
| Compound Annual Growth Rate | 7.3% |
| Regions Covered | Global |