Global Healthcare RCM Outsourcing Market - Key Trends and Drivers Summarized
Why Is Revenue Cycle Management Becoming Essential for Maximizing Financial Performance, Streamlining Billing Processes, and Enhancing Healthcare Operations?
Revenue cycle management (RCM) has become essential for maximizing financial performance, streamlining billing processes, and enhancing healthcare operations in today's healthcare industry. But why is it so critical now? Healthcare providers face increasing financial pressures due to rising costs, regulatory changes, and the complexity of insurance claims processing. RCM provides the structure needed to manage the entire financial lifecycle of a patient's healthcare experience - from appointment scheduling and patient registration to billing, claims processing, and payment collection. By efficiently managing these processes, healthcare organizations can optimize revenue flow, minimize claim denials, and ensure they receive timely payments for services rendered.Effective revenue cycle management ensures that healthcare organizations can track and manage their financial performance in real-time. By automating billing and coding processes, reducing errors in claims submission, and ensuring compliance with payer requirements, RCM improves the efficiency of financial operations. This results in faster reimbursements, fewer delays in payment, and improved cash flow. Additionally, by handling insurance verification, eligibility checks, and pre-authorizations, RCM helps reduce the risk of rejected or denied claims, ensuring that healthcare providers receive payment for the services they provide.
RCM also plays a critical role in enhancing healthcare operations by freeing up administrative staff from manual billing tasks. With efficient RCM systems, staff can focus more on patient care and less on chasing payments or resolving billing disputes. Furthermore, by offering real-time insights into financial performance, RCM helps healthcare organizations make data-driven decisions to improve resource allocation, reduce operational inefficiencies, and ensure financial sustainability.
How Are Technological Advancements and Innovations Improving the Accuracy, Efficiency, and Security of Revenue Cycle Management?
Technological advancements and innovations are significantly improving the accuracy, efficiency, and security of revenue cycle management, making it more effective for healthcare organizations to manage their financial processes. One of the most impactful innovations is the integration of automation and artificial intelligence (AI) into RCM systems. Automation tools, such as robotic process automation (RPA), streamline repetitive tasks like claims submission, insurance verification, and patient billing. By automating these processes, healthcare organizations can reduce the administrative burden, minimize human errors, and improve the speed of payment collections. AI-powered systems take this a step further by analyzing billing data to identify discrepancies, predict claim denials, and optimize coding accuracy, ensuring that claims are processed correctly the first time.Another significant advancement in RCM is the widespread adoption of cloud-based platforms. Cloud-based RCM systems allow healthcare organizations to centralize their billing, claims, and payment processes, making it easier to access and manage financial data from anywhere. Cloud solutions also enhance scalability, enabling healthcare providers to expand their RCM operations as they grow, without needing to invest heavily in on-premises infrastructure. Cloud-based systems are also more secure, offering encryption, multi-factor authentication, and real-time monitoring to protect sensitive patient financial information from cyber threats and data breaches.
Machine learning (ML) and predictive analytics are also transforming RCM by improving the accuracy of revenue forecasts and identifying trends in claim denials. By analyzing historical claims data, ML algorithms can predict which claims are likely to be denied and suggest corrective actions to prevent rejections. This not only reduces claim denials but also shortens the payment cycle, leading to faster reimbursements and improved financial performance. Predictive analytics also allows healthcare organizations to optimize their financial strategies by providing insights into revenue trends, patient payment behavior, and insurance payer performance.
Blockchain technology is emerging as a powerful tool for enhancing the security and transparency of revenue cycle management. Blockchain offers a decentralized ledger that records and verifies all financial transactions in a tamper-proof and auditable format. This ensures that healthcare organizations have a transparent and secure record of claims, payments, and contract agreements with insurers, reducing the risk of disputes and fraud. Blockchain can also streamline the verification process for claims and payments by ensuring that all parties involved - providers, payers, and patients - have access to a single, immutable record of the transaction, which improves trust and accountability across the healthcare ecosystem.
Electronic health records (EHR) integration with RCM systems is another key technological advancement. By linking patient clinical data with billing information, healthcare providers can ensure that coding and billing are accurate and reflect the services provided. This integration reduces errors in claims submissions, increases coding accuracy, and helps avoid delays caused by incomplete or inaccurate information. Moreover, EHR integration improves the patient experience by ensuring that billing and payment processes are aligned with clinical care, allowing for more transparent and understandable bills.
Why Is Revenue Cycle Management Critical for Reducing Claim Denials, Improving Cash Flow, and Enhancing Patient Satisfaction?
Revenue cycle management is critical for reducing claim denials, improving cash flow, and enhancing patient satisfaction because it provides healthcare organizations with the tools and processes needed to manage financial operations efficiently and effectively. One of the primary reasons RCM is so valuable is its ability to reduce claim denials. Claim denials are one of the biggest challenges facing healthcare providers, leading to delayed payments and revenue loss. RCM systems help prevent denials by automating the verification of insurance eligibility, ensuring proper coding, and checking claims for errors before they are submitted. This proactive approach reduces the likelihood of denials, minimizes rework, and speeds up the payment process.Improving cash flow is another significant benefit of effective revenue cycle management. By automating billing processes and reducing the time it takes to submit claims and receive payments, RCM helps healthcare organizations maintain a steady cash flow. This is crucial for financial sustainability, especially in today's healthcare environment where providers face increasing costs and reimbursement pressures. RCM systems also improve payment collection by streamlining patient billing and offering flexible payment options, such as online payment portals or automated payment plans. These options make it easier for patients to pay their bills, reducing the risk of bad debt and improving overall revenue collection.
Enhancing patient satisfaction is another key function of revenue cycle management. Patients often experience frustration with healthcare billing, particularly when they receive unexpected or confusing bills. RCM systems help address these issues by providing clear, transparent billing processes. Patients can receive detailed explanations of their bills, including what their insurance covers, what they owe, and payment options. Offering this level of transparency and communication helps build trust with patients, improving their overall experience. Furthermore, by ensuring that claims are processed accurately and quickly, RCM reduces the likelihood of billing errors, disputes, and delays, all of which contribute to better patient satisfaction.
RCM also plays a vital role in supporting patient financial engagement. In today's healthcare landscape, patients are increasingly responsible for a larger portion of their healthcare costs, including copayments, deductibles, and coinsurance. RCM systems help healthcare organizations engage patients early in the billing process by providing upfront cost estimates, explaining payment responsibilities, and offering payment options before services are rendered. This proactive approach not only improves patient satisfaction but also increases the likelihood of timely payments.
Moreover, revenue cycle management enhances operational efficiency by streamlining administrative tasks and reducing manual workloads. By automating claims submissions, payment tracking, and reporting processes, RCM allows healthcare providers to focus more on patient care and less on financial administration. This leads to better use of staff resources, lower administrative costs, and improved overall efficiency in healthcare operations.
What Factors Are Driving the Growth of the Revenue Cycle Management Market?
Several key factors are driving the rapid growth of the revenue cycle management market, including the increasing complexity of healthcare billing, the shift toward value-based care, the rise in patient financial responsibility, and advancements in digital health technologies. One of the primary drivers is the growing complexity of healthcare billing and insurance claims processes. As healthcare providers navigate various payer policies, reimbursement models, and regulatory requirements, the need for sophisticated RCM solutions has become more urgent. RCM systems help healthcare organizations manage the intricacies of billing, coding, and claims submissions while ensuring compliance with changing regulations, such as those related to Medicare, Medicaid, and the Affordable Care Act.The shift toward value-based care is another major factor fueling the growth of the RCM market. Value-based care models focus on delivering high-quality care while controlling costs, and these models require more detailed tracking of outcomes, costs, and payments. RCM systems play a critical role in supporting value-based care by ensuring that providers are reimbursed based on patient outcomes and quality of care, rather than the volume of services provided. These systems help healthcare organizations track performance metrics, manage contracts with payers, and ensure that payments align with value-based reimbursement models.
The rise in patient financial responsibility is also contributing to the growth of the RCM market. As patients become responsible for a larger share of their healthcare costs due to high-deductible health plans and increased out-of-pocket expenses, healthcare providers must manage patient payments more effectively. RCM systems help healthcare organizations engage patients in the financial process by providing clear billing information, offering cost estimates, and allowing flexible payment options. These tools are essential for improving patient payment collections and reducing bad debt, which has become a growing concern for healthcare providers.
Advancements in digital health technologies are further accelerating the growth of the RCM market. Innovations such as cloud computing, AI, automation, and data analytics are making RCM systems more powerful, scalable, and user-friendly. Cloud-based RCM solutions allow healthcare organizations to manage billing and claims processes more efficiently by providing real-time access to financial data, automating claims submissions, and enabling seamless communication between healthcare providers and payers. AI and predictive analytics are improving the accuracy of claims processing by identifying potential errors or denials before claims are submitted, reducing rework and speeding up reimbursements. These technological advancements are driving the adoption of RCM systems across healthcare organizations of all sizes.
Regulatory changes and government initiatives aimed at improving healthcare transparency and efficiency are also driving the adoption of revenue cycle management solutions. For example, regulations requiring healthcare providers to offer cost transparency, comply with electronic claims submission standards, and adhere to strict data security protocols are pushing organizations to invest in more sophisticated RCM tools. Additionally, government initiatives aimed at expanding access to healthcare, such as Medicaid expansion, have increased the complexity of payer relationships, making RCM systems essential for managing the growing volume of claims and payments.
In conclusion, the growth of the revenue cycle management market is driven by the increasing complexity of healthcare billing, the rise of value-based care models, growing patient financial responsibility, and advancements in digital health technologies. As healthcare providers continue to face financial pressures and evolving payment models, revenue cycle management systems will play an increasingly critical role in ensuring financial sustainability, improving cash flow, and enhancing patient satisfaction.
Report Scope
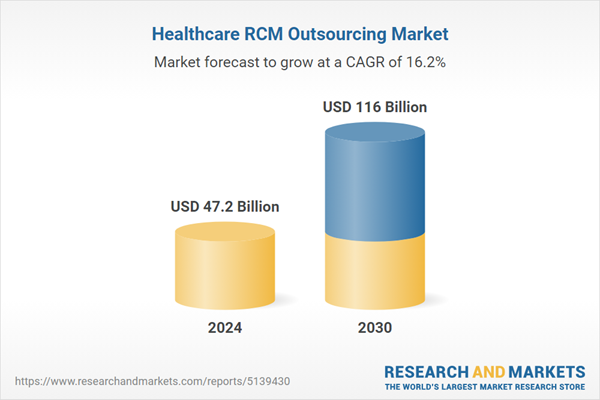
The report analyzes the Healthcare RCM Outsourcing market, presented in terms of market value (USD). The analysis covers the key segments and geographic regions outlined below.- Segments: Service (Back-End Services, Middle Services, Front-End Services); Type (Pre-Intervention, Intervention, Post-Intervention); End-Use (Hospitals, Other End-Uses).
- Geographic Regions/Countries: World; United States; Canada; Japan; China; Europe (France; Germany; Italy; United Kingdom; and Rest of Europe); Asia-Pacific; Rest of World.
Key Insights:
- Market Growth: Understand the significant growth trajectory of the Pre-Intervention Type segment, which is expected to reach US$44.8 Billion by 2030 with a CAGR of 14.5%. The Intervention Type segment is also set to grow at 16.8% CAGR over the analysis period.
- Regional Analysis: Gain insights into the U.S. market, valued at $13.1 Billion in 2024, and China, forecasted to grow at an impressive 15.4% CAGR to reach $17.7 Billion by 2030. Discover growth trends in other key regions, including Japan, Canada, Germany, and the Asia-Pacific.
Why You Should Buy This Report:
- Detailed Market Analysis: Access a thorough analysis of the Global Healthcare RCM Outsourcing Market, covering all major geographic regions and market segments.
- Competitive Insights: Get an overview of the competitive landscape, including the market presence of major players across different geographies.
- Future Trends and Drivers: Understand the key trends and drivers shaping the future of the Global Healthcare RCM Outsourcing Market.
- Actionable Insights: Benefit from actionable insights that can help you identify new revenue opportunities and make strategic business decisions.
Key Questions Answered:
- How is the Global Healthcare RCM Outsourcing Market expected to evolve by 2030?
- What are the main drivers and restraints affecting the market?
- Which market segments will grow the most over the forecast period?
- How will market shares for different regions and segments change by 2030?
- Who are the leading players in the market, and what are their prospects?
Report Features:
- Comprehensive Market Data: Independent analysis of annual sales and market forecasts in US$ Million from 2024 to 2030.
- In-Depth Regional Analysis: Detailed insights into key markets, including the U.S., China, Japan, Canada, Europe, Asia-Pacific, Latin America, Middle East, and Africa.
- Company Profiles: Coverage of players such as Accretive Health (R1 RCM Inc), Allscripts Healthcare Solutions, Inc., Availity, Cerner, Change Healthcare (Emdeon) and more.
- Complimentary Updates: Receive free report updates for one year to keep you informed of the latest market developments.
Some of the 36 companies featured in this Healthcare RCM Outsourcing market report include:
- Accretive Health (R1 RCM Inc)
- Allscripts Healthcare Solutions, Inc.
- Availity
- Cerner
- Change Healthcare (Emdeon)
- Conifer Health Solutions
- Emdeon Business Services
- GeBBS Healthcare
- McKesson
- MedAssets
- MedAssist (Firstsource)
- MedData (Cardon Outreach)
- nthrive (Medassets + Precyse)
- optum360
- Parallon Business Solutions
- The SSI Group
This edition integrates the latest global trade and economic shifts into comprehensive market analysis. Key updates include:
- Tariff and Trade Impact: Insights into global tariff negotiations across 180+ countries, with analysis of supply chain turbulence, sourcing disruptions, and geographic realignment. Special focus on 2025 as a pivotal year for trade tensions, including updated perspectives on the Trump-era tariffs.
- Adjusted Forecasts and Analytics: Revised global and regional market forecasts through 2030, incorporating tariff effects, economic uncertainty, and structural changes in globalization. Includes historical analysis from 2015 to 2023.
- Strategic Market Dynamics: Evaluation of revised market prospects, regional outlooks, and key economic indicators such as population and urbanization trends.
- Innovation & Technology Trends: Latest developments in product and process innovation, emerging technologies, and key industry drivers shaping the competitive landscape.
- Competitive Intelligence: Updated global market share estimates for 2025, competitive positioning of major players (Strong/Active/Niche/Trivial), and refined focus on leading global brands and core players.
- Expert Insight & Commentary: Strategic analysis from economists, trade experts, and domain specialists to contextualize market shifts and identify emerging opportunities.
Table of Contents
Companies Mentioned (Partial List)
A selection of companies mentioned in this report includes, but is not limited to:
- Accretive Health (R1 RCM Inc)
- Allscripts Healthcare Solutions, Inc.
- Availity
- Cerner
- Change Healthcare (Emdeon)
- Conifer Health Solutions
- Emdeon Business Services
- GeBBS Healthcare
- McKesson
- MedAssets
- MedAssist (Firstsource)
- MedData (Cardon Outreach)
- nthrive (Medassets + Precyse)
- optum360
- Parallon Business Solutions
- The SSI Group
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 241 |
| Published | February 2026 |
| Forecast Period | 2024 - 2030 |
| Estimated Market Value ( USD | $ 47.2 Billion |
| Forecasted Market Value ( USD | $ 116 Billion |
| Compound Annual Growth Rate | 16.2% |
| Regions Covered | Global |