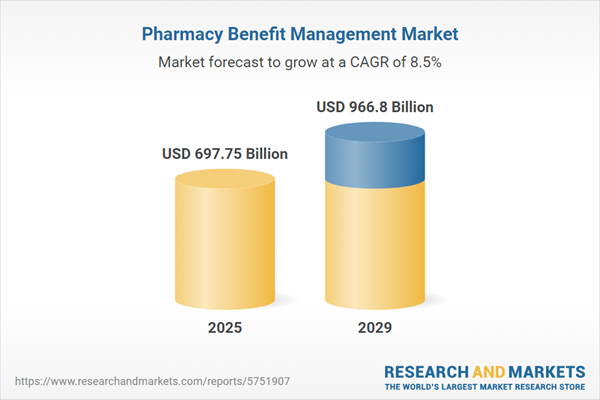
The pharmacy benefit management market size is expected to see strong growth in the next few years. It will grow to $966.8 billion in 2029 at a compound annual growth rate (CAGR) of 8.5%. The growth in the forecast period can be attributed to healthcare cost control demands, rise in prescription drug usage, health insurance expansion, adherence to regulatory changes, patient-centric healthcare. Major trends in the forecast period include value-based healthcare models, specialty medications management, data analytics and AI integration, telemedicine integration, rise in personalized medicine.
The increase in the number of individuals obtaining insurance is a significant driver for the growth of the pharmacy benefit management (PBM) market. Insurance helps address rising medical expenses by covering costs associated with treatments, hospital stays, health check-ups, and other related medical expenditures. Likewise, PBM provides comprehensive healthcare product support by integrating both medical and pharmaceutical services. This approach offers insurers detailed insights into patient data, enabling them to deliver effective programs to patients. For example, the United States Department of Health and Human Services, a cabinet-level department of the U.S. federal government, reported a 31% increase in coverage sign-ups, with 5.1 million additional consumers enrolling during the 2024 Open Enrollment Period (OEP) compared to the 2023 OEP. Consequently, the rise in insurance uptake is fueling the growth of the pharmacy benefit management market.
The escalating prevalence of chronic diseases is anticipated to drive the growth of the pharmacy benefit management (PBM) market in the coming years. Chronic diseases, characterized by long-term health conditions persisting for three months or more, pose a significant global health challenge. Pharmacy benefit management is instrumental in the effective management of chronic diseases by optimizing medication access, fostering adherence, and implementing cost-effective strategies. This approach ensures improved health outcomes and a higher quality of life for individuals dealing with long-term medical conditions. As of September 2023, the World Health Organization (WHO) reported that noncommunicable diseases (NCDs) or chronic diseases accounted for 74% of the 41 million annual global deaths. Notably, this figure includes 17.9 million deaths attributed to cardiovascular diseases, 9.3 million to cancer, 4.1 million to chronic respiratory diseases, and 2 million to diabetes. Consequently, the rising prevalence of chronic diseases stands as a significant factor propelling the growth of the pharmacy benefit management market.
Leading companies in the pharmacy benefit management (PBM) market are prioritizing acquisitions and partnerships to increase market share. Such deals enable companies to broaden their product portfolios and drive higher sales. For example, in December 2022, Prime Therapeutics LLC, a U.S.-based pharmacy solutions company specializing in PBM, acquired Magellan Rx Management for $1.35 billion, integrating its PBM services with specialty drug management expertise. This acquisition aims to expand service offerings, boost affordability, improve patient care, increase membership, and maintain operational independence. The acquisition aligns with the healthcare sector's 'Quadruple Aim' goals, strengthening Prime Therapeutics’ PBM platform. Magellan Rx Management, also U.S.-based, specializes in comprehensive pharmacy and medical benefits management.
Prominent companies in the PBM market are also introducing digital prescription technologies to enhance prescription drug cost management. Digital prescription technology involves electronic systems to create, transmit, store, and manage medication prescriptions. For instance, in August 2024, UNC Health, a U.S.-based medical system, launched UNC Health Pharmacy Solutions, an advanced PBM platform blending clinical excellence with a transparent model for prescription cost management. The platform offers up to 32% in total savings along with comprehensive pharmacy services and has achieved a Net Promoter Score of 95. UNC Health aims to be the preferred PBM in North and South Carolina, helping partners reduce overall care costs and improve member outcomes. The program utilizes dynamic plan management, unique strategies for biosimilars and weight-loss medications, and individualized consultations with clinical pharmacists.
In January 2022, Centene, a prominent US-based managed care company specializing in healthcare solutions for individuals and families, successfully completed the acquisition of Magellan, a leading US-based entity renowned for its expertise in managing the most rapidly expanding and intricate segments of the healthcare industry. This strategic transaction, valued at $2.2 billion, positions Centene to deliver comprehensive, integrated healthcare solutions tailored for complex, high-cost populations. The acquisition aims to enhance health outcomes while concurrently achieving cost efficiencies within this specialized sector.
Major companies operating in the pharmacy benefit management market include CVS Health Corporation, Cigna Corporation, Centene Corporation, Anthem Inc., OptumRx Inc., Humana Pharmacy Solutions Inc., Magellan Health Inc., Prime Therapeutics LLC, MaxorPlus Ltd., RxAdvance Corp, MedImpact Healthcare Systems Inc., PerformRx LLC., Navitus Health Solutions LLC, WellDyneRx Inc., Healthesystems LLC., Catalyst Rx Inc., Argus Health Systems Inc., Innoviant Pharmacy Inc., Pharmaceutical Strategies Group, ProCare Rx Inc., FutureScripts LLC., National CooperativeRx, ScriptCare Ltd., US Script Inc., LDI Integrated Pharmacy Services LLC, RxPreferred Benefits, SinfoníaRx Inc.
North America was the largest region in the pharmacy benefit management market in 2024. Asia-Pacific is expected to be the fastest-growing region in the forecast period. The regions covered in the pharmacy benefit management market report are Asia-Pacific, Western Europe, Eastern Europe, North America, South America, Middle East, Africa. The countries covered in the pharmacy benefit management market report are Australia, Brazil, China, France, Germany, India, Indonesia, Japan, Russia, South Korea, UK, USA, Canada, Italy, Spain.
Pharmacy benefit management refers to a network of businesses acting as intermediaries between insurance companies, pharmacies, and drug distributors. Its primary purpose is to facilitate the negotiation process between insurers and pharmaceutical companies, aiming to secure reduced prescription costs.
The primary services offered by pharmacy benefit management (PBM) include mail-delivery, specialty pharmacy, and preferred network pharmacy. Mail-delivery involves the direct shipment of medicines to the desired location through mail-order delivery services. These services are extended across various types of PBMs, which include commercial health plans, self-insured employer plans, Medicare Part D plans, and the Federal Employees Health Benefits Program. Different types of PBMs serve major end-users, including pharmacy benefit management organizations, mail-order pharmacies, retail pharmacies, inpatient pharmacies, and outpatient pharmacies, catering to diverse needs within the healthcare sector.
The pharmacy benefit management market research report is one of a series of new reports that provides pharmacy benefit management market statistics, including pharmacy benefit management industry global market size, regional shares, competitors with a pharmacy benefit management market share, detailed pharmacy benefit management market segments, market trends and opportunities, and any further data you may need to thrive in the pharmacy benefit management industry. This pharmacy benefit management market research report delivers a complete perspective of everything you need, with an in-depth analysis of the current and future scenarios of the industry.
The pharmacy benefit management market includes revenues earned by entities by providing case management, disease management, and drug utilization services. The market value includes the value of related goods sold by the service provider or included within the service offering. Only goods and services traded between entities or sold to end consumers are included.
The market value is defined as the revenues that enterprises gain from the sale of goods and/or services within the specified market and geography through sales, grants, or donations in terms of the currency (in USD, unless otherwise specified).
The revenues for a specified geography are consumption values that are revenues generated by organizations in the specified geography within the market, irrespective of where they are produced. It does not include revenues from resales along the supply chain, either further along the supply chain or as part of other products.
This product will be delivered within 3-5 business days.
Table of Contents
Executive Summary
Pharmacy Benefit Management Global Market Report 2025 provides strategists, marketers and senior management with the critical information they need to assess the market.This report focuses on pharmacy benefit management market which is experiencing strong growth. The report gives a guide to the trends which will be shaping the market over the next ten years and beyond.
Reasons to Purchase:
- Gain a truly global perspective with the most comprehensive report available on this market covering 15 geographies.
- Assess the impact of key macro factors such as conflict, pandemic and recovery, inflation and interest rate environment and the 2nd Trump presidency.
- Create regional and country strategies on the basis of local data and analysis.
- Identify growth segments for investment.
- Outperform competitors using forecast data and the drivers and trends shaping the market.
- Understand customers based on the latest market shares.
- Benchmark performance against key competitors.
- Suitable for supporting your internal and external presentations with reliable high quality data and analysis
- Report will be updated with the latest data and delivered to you along with an Excel data sheet for easy data extraction and analysis.
- All data from the report will also be delivered in an excel dashboard format.
Description
Where is the largest and fastest growing market for pharmacy benefit management? How does the market relate to the overall economy, demography and other similar markets? What forces will shape the market going forward? The pharmacy benefit management market global report answers all these questions and many more.The report covers market characteristics, size and growth, segmentation, regional and country breakdowns, competitive landscape, market shares, trends and strategies for this market. It traces the market’s historic and forecast market growth by geography.
- The market characteristics section of the report defines and explains the market.
- The market size section gives the market size ($b) covering both the historic growth of the market, and forecasting its development.
- The forecasts are made after considering the major factors currently impacting the market. These include:
- The forecasts are made after considering the major factors currently impacting the market. These include the Russia-Ukraine war, rising inflation, higher interest rates, and the legacy of the COVID-19 pandemic.
- Market segmentations break down the market into sub markets.
- The regional and country breakdowns section gives an analysis of the market in each geography and the size of the market by geography and compares their historic and forecast growth. It covers the growth trajectory of COVID-19 for all regions, key developed countries and major emerging markets.
- The competitive landscape chapter gives a description of the competitive nature of the market, market shares, and a description of the leading companies. Key financial deals which have shaped the market in recent years are identified.
- The trends and strategies section analyses the shape of the market as it emerges from the crisis and suggests how companies can grow as the market recovers.
Scope
Markets Covered:
1) By Services: Mail-Delivery, Specialty Pharmacy, Preferred Network Pharmacy2) By Type: Commercial Health Plans, Self-Insured Employer Plans, Medicare Part D Plans, Federal Employees Health Benefits Program
3) By End User: Pharmacy Benefit Management Organization, Mail Order Pharmacies, Retail Pharmacies, Inpatient Pharmacies, Outpatient Pharmacies
Subsegments:
1) By Mail-Delivery: Maintenance Medications; Acute Care Medications; Patient Education and Support Services2) By Specialty Pharmacy: High-Cost Medications; Biologics and Biosimilars; Disease Management Services
3) By Preferred Network Pharmacy: Retail Pharmacy Networks; Contracted Pharmacy Networks; Urgent Care Pharmacy Services
Key Companies Mentioned: CVS Health Corporation; Cigna Corporation; Centene Corporation; Anthem Inc.; OptumRx Inc.
Countries: Australia; Brazil; China; France; Germany; India; Indonesia; Japan; Russia; South Korea; UK; USA; Canada; Italy; Spain
Regions: Asia-Pacific; Western Europe; Eastern Europe; North America; South America; Middle East; Africa
Time Series: Five years historic and ten years forecast.
Data: Ratios of market size and growth to related markets, GDP proportions, expenditure per capita.
Data Segmentation: Country and regional historic and forecast data, market share of competitors, market segments.
Sourcing and Referencing: Data and analysis throughout the report is sourced using end notes.
Delivery Format: PDF, Word and Excel Data Dashboard.
Companies Mentioned
- CVS Health Corporation
- Cigna Corporation
- Centene Corporation
- Anthem Inc.
- OptumRx Inc.
- Humana Pharmacy Solutions Inc.
- Magellan Health Inc.
- Prime Therapeutics LLC
- MaxorPlus Ltd.
- RxAdvance Corp
- MedImpact Healthcare Systems Inc.
- PerformRx LLC.
- Navitus Health Solutions LLC
- WellDyneRx Inc.
- Healthesystems LLC.
- Catalyst Rx Inc.
- Argus Health Systems Inc.
- Innoviant Pharmacy Inc.
- Pharmaceutical Strategies Group
- ProCare Rx Inc.
- FutureScripts LLC.
- National CooperativeRx
- ScriptCare Ltd.
- US Script Inc.
- LDI Integrated Pharmacy Services LLC
- RxPreferred Benefits
- SinfoníaRx Inc.
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 200 |
| Published | March 2025 |
| Forecast Period | 2025 - 2029 |
| Estimated Market Value ( USD | $ 697.75 Billion |
| Forecasted Market Value ( USD | $ 966.8 Billion |
| Compound Annual Growth Rate | 8.5% |
| Regions Covered | Global |
| No. of Companies Mentioned | 27 |