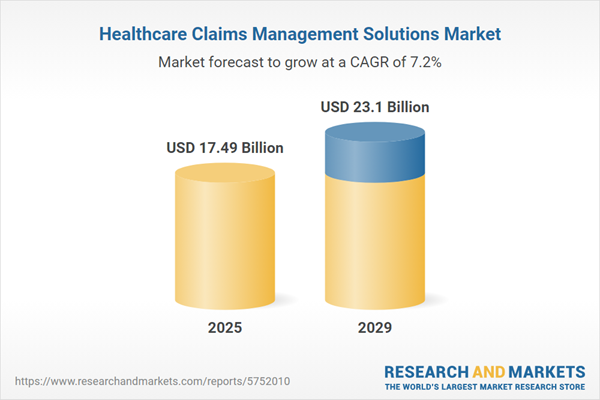
The healthcare claims management solutions market size has grown strongly in recent years. It will grow from $16.45 billion in 2024 to $17.49 billion in 2025 at a compound annual growth rate (CAGR) of 6.3%. The growth in the historic period can be attributed to increased healthcare cost, regulatory compliance, paperless claims processing, improved accuracy, provider-payer collaboration.
The healthcare claims management solutions market size is expected to see strong growth in the next few years. It will grow to $23.1 billion in 2029 at a compound annual growth rate (CAGR) of 7.2%. The growth in the forecast period can be attributed to telehealth expansion, value-based care, interoperability, cybersecurity, pandemic preparedness. Major trends in the forecast period include blockchain for claims processing, ai-powered claims analytics, predictive analytics for fraud detection, mobile claims submission:, automated claims adjudication.
The rapid increase in the ageing population is anticipated to drive the growth of the healthcare claims management solutions market. The ageing population, referring to individuals aged 65 and over, requires streamlined processes for healthcare claims to expedite the payment lifecycle. Healthcare claims management solutions offer easier access to claim management, meeting the demands of an ageing population. As reported by the World Health Organization in October 2022, globally, 1 in 6 individuals is projected to be 60 or older by 2030, reaching an expected 2.1 billion elderly people by 2050. This demographic shift is identified as a significant driver propelling the healthcare claims management market.
The increasing incidence of chronic diseases is expected to contribute to the growth of the healthcare claims management solutions market. Chronic diseases, which persist over an extended period, necessitate ongoing medical management. Healthcare claims management solutions play a crucial role in supporting the efficient and accurate processing of claims, ensuring timely reimbursement for healthcare providers offering chronic disease management services. Projections from the National Center for Biotechnology Information (NCBI) in January 2023 indicate that by the year 2050, the number of individuals aged 50 years and older with at least one chronic illness is expected to surge by 99.5%, from 71.522 million in 2020 to 142.66 million. This growing incidence of chronic diseases is identified as a key factor propelling the healthcare claims management solutions market.
Advancements in technology for innovative treatments in healthcare represent a key trend gaining popularity in the healthcare claims management solutions market. Major companies operating in this sector are actively introducing new technologies to provide innovative treatments, contributing to the sustainability of their positions in the market. For example, in January 2022, Treatment.com International Inc., a US-based healthcare software solutions provider, including healthcare claims management, launched the Treatment Digital Health App. This doctor-built digital health app utilizes AI software technology to provide users with wide access to highly accurate insights about their health, offering diagnoses and customized treatments. This integration of technology and healthcare solutions reflects the industry's commitment to innovation in providing enhanced patient care through healthcare claims management solutions.
Leading companies in the healthcare claims management solutions market are actively focusing on product innovation, exemplified by the introduction of AI-enabled solutions such as the Claims Data Activator Suite, to sustain their positions in the market. The Claims Data Activator Suite aims to establish data interoperability, intelligent analytics, and smart reporting by leveraging technologies such as Document AI, the Healthcare Natural Language API, and the Healthcare API. This innovation enables the transformation of unstructured data into structured data, offering enhanced capabilities for healthcare claims management. In April 2023, Google LLC, a major US-based technology company, launched a new Google Cloud AI-enabled claims data activator. This solution is designed to assist health plans and providers in reducing administrative costs and responsibilities by converting unstructured data into structured data. The Claims Data Activator empowers specialists to make quicker, better-informed decisions, ultimately improving patient care.
In February 2022, Hellman & Friedman, a prominent US-based private equity firm, and Bain Capital, a leading US-based private investment firm, made a significant move by acquiring Athenahealth for a deal amount of $17 billion. This strategic acquisition positions Hellman & Friedman and Bain Capital with the largest and most innovative provider of cloud-based electronic medical records and physician practice solutions across the healthcare industry. Athenahealth, a US-based healthcare technology provider, operates in the healthcare claims management solutions market. This acquisition reflects the industry's strategic focus on partnerships and acquisitions to strengthen capabilities and offerings, emphasizing the importance of innovative solutions in healthcare claims management.
Major companies operating in the healthcare claims management solutions market include Allscripts Healthcare Solutions Inc., Athenahealth, McKesson Corporation, Oracle Corporation, Alpha II LLC, Availity Co., Cerner Corporation, Change Healthcare, Conifer Health Solutions LLC, eClinicalWorks, EmblemHealth Co., Emdeon Inc., Epic Systems Corporation, Inovalon Co., InstaMed Co., Kareo Co., NaviNet Inc., NTT Data Services, Optum Inc., Provation Medical, SSI Group LLC, The SSI Group, Cognizant Technology Ltd., TruBridge Co., Waystar Co., ZirMed Inc.
North America was the largest region in the healthcare claim management solution market in 2024. Asia-Pacific is expected to be the fastest-growing region in the forecast period. The regions covered in the healthcare claim management solution market share report are Asia-Pacific, Western Europe, Eastern Europe, North America, South America, Middle East, and Africa. The countries covered in the healthcare claim management solution market report are Australia, Brazil, China, France, Germany, India, Indonesia, Japan, Russia, South Korea, UK and USA.
Healthcare claims management solutions aim to achieve comprehensive automation of claims processing, ensuring rapid access to client information while maintaining the confidentiality of private medical data.
The primary categories of healthcare claims management solutions include software and services. Software encompasses a set of data, instructions, or programs utilized in computers to execute specific tasks. Deployment methods include web-based, cloud-based, and on-premise solutions. These solutions cater to various end-users, including healthcare payers, healthcare providers, and other entities.
The healthcare claims management solutions market research report is one of a series of new reports that provides healthcare claims management solutions market statistics, including healthcare claims management solutions industry global market size, regional shares, competitors with a healthcare claims management solutions market share, detailed healthcare claims management solutions market segments, market trends and opportunities, and any further data you may need to thrive in the healthcare claims management solutions industry. This healthcare claims management solutions market research report delivers a complete perspective of everything you need, with an in-depth analysis of the current and future scenario of the industry.
The healthcare claims management solutions market consists of sales of healthcare software and related services. Values in this market are ‘factory gate’ values, that is the value of goods sold by the manufacturers or creators of the goods, whether to other entities (including downstream manufacturers, wholesalers, distributors and retailers) or directly to end customers. The value of goods in this market includes related services sold by the creators of the goods.
The market value is defined as the revenues that enterprises gain from the sale of goods and/or services within the specified market and geography through sales, grants, or donations in terms of the currency (in USD unless otherwise specified).
The revenues for a specified geography are consumption values that are revenues generated by organizations in the specified geography within the market, irrespective of where they are produced. It does not include revenues from resales along the supply chain, either further along the supply chain or as part of other products.
This product will be delivered within 3-5 business days.
Table of Contents
Executive Summary
Healthcare Claims Management Solutions Global Market Report 2025 provides strategists, marketers and senior management with the critical information they need to assess the market.This report focuses on healthcare claims management solutions market which is experiencing strong growth. The report gives a guide to the trends which will be shaping the market over the next ten years and beyond.
Reasons to Purchase:
- Gain a truly global perspective with the most comprehensive report available on this market covering 15 geographies.
- Assess the impact of key macro factors such as conflict, pandemic and recovery, inflation and interest rate environment and the 2nd Trump presidency.
- Create regional and country strategies on the basis of local data and analysis.
- Identify growth segments for investment.
- Outperform competitors using forecast data and the drivers and trends shaping the market.
- Understand customers based on the latest market shares.
- Benchmark performance against key competitors.
- Suitable for supporting your internal and external presentations with reliable high quality data and analysis
- Report will be updated with the latest data and delivered to you along with an Excel data sheet for easy data extraction and analysis.
- All data from the report will also be delivered in an excel dashboard format.
Description
Where is the largest and fastest growing market for healthcare claims management solutions? How does the market relate to the overall economy, demography and other similar markets? What forces will shape the market going forward? The healthcare claims management solutions market global report answers all these questions and many more.The report covers market characteristics, size and growth, segmentation, regional and country breakdowns, competitive landscape, market shares, trends and strategies for this market. It traces the market’s historic and forecast market growth by geography.
- The market characteristics section of the report defines and explains the market.
- The market size section gives the market size ($b) Covering both the historic growth of the market, and forecasting its development.
- The forecasts are made after considering the major factors currently impacting the market. These include:
- The forecasts are made after considering the major factors currently impacting the market. These include the Russia-Ukraine war, rising inflation, higher interest rates, and the legacy of the COVID-19 pandemic.
- Market segmentations break down the market into sub markets.
- The regional and country breakdowns section gives an analysis of the market in each geography and the size of the market by geography and compares their historic and forecast growth. It covers the growth trajectory of COVID-19 for all regions, key developed countries and major emerging markets.
- The competitive landscape chapter gives a description of the competitive nature of the market, market shares, and a description of the leading companies. Key financial deals which have shaped the market in recent years are identified.
- The trends and strategies section analyses the shape of the market as it emerges from the crisis and suggests how companies can grow as the market recovers.
Scope
Markets Covered:
1) By Type: Software; Services2) By Deployment Mode: Web-Based; Cloud-Based; on-Premise
3) By End-User: Healthcare Payers; Healthcare Providers; Other End-Users
Subsegments:
1) By Software: Claims Processing Software; Revenue Cycle Management Software; Medical Billing Software; Analytics and Reporting Tools2) By Services: Consulting Services; Implementation Services; Training and Support Services; Claims Auditing Services
Key Companies Mentioned: Allscripts Healthcare Solutions Inc.; Athenahealth; McKesson Corporation; Oracle Corporation; Alpha II LLC
Countries: Australia; Brazil; China; France; Germany; India; Indonesia; Japan; Russia; South Korea; UK; USA; Canada; Italy; Spain
Regions: Asia-Pacific; Western Europe; Eastern Europe; North America; South America; Middle East; Africa
Time Series: Five years historic and ten years forecast.
Data: Ratios of market size and growth to related markets, GDP proportions, expenditure per capita.
Data Segmentation: Country and regional historic and forecast data, market share of competitors, market segments.
Sourcing and Referencing: Data and analysis throughout the report is sourced using end notes.
Delivery Format: PDF, Word and Excel Data Dashboard.
Companies Mentioned
Some of the major companies featured in this Healthcare Claims Management Solutions market report include:- Allscripts Healthcare Solutions Inc.
- Athenahealth
- McKesson Corporation
- Oracle Corporation
- Alpha II LLC
- Availity Co.
- Cerner Corporation
- Change Healthcare
- Conifer Health Solutions LLC
- eClinicalWorks
- EmblemHealth Co.
- Emdeon Inc.
- Epic Systems Corporation
- Inovalon Co.
- InstaMed Co.
- Kareo Co.
- NaviNet Inc.
- NTT Data Services
- Optum Inc.
- Provation Medical
- SSI Group LLC
- The SSI Group
- Cognizant Technology Ltd.
- TruBridge Co.
- Waystar Co.
- ZirMed Inc.
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 200 |
| Published | February 2025 |
| Forecast Period | 2025 - 2029 |
| Estimated Market Value ( USD | $ 17.49 Billion |
| Forecasted Market Value ( USD | $ 23.1 Billion |
| Compound Annual Growth Rate | 7.2% |
| Regions Covered | Global |
| No. of Companies Mentioned | 26 |