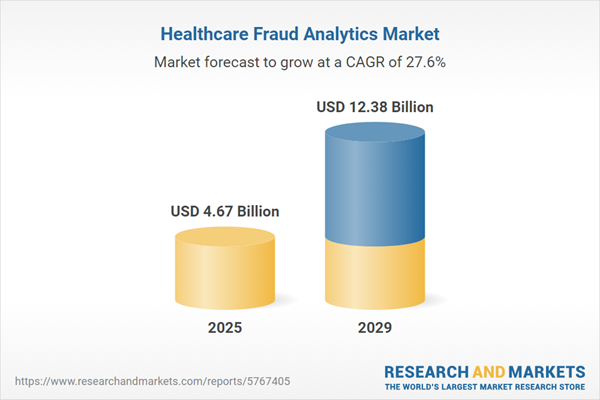
The healthcare fraud analytics market size has grown exponentially in recent years. It will grow from $3.73 billion in 2024 to $4.67 billion in 2025 at a compound annual growth rate (CAGR) of 25.4%. The growth in the historic period can be attributed to rise in healthcare costs, complexity of healthcare systems, increasing volume of healthcare data, transition to electronic health records (EHRs), billing fraud challenges.
The healthcare fraud analytics market size is expected to see exponential growth in the next few years. It will grow to $12.38 billion in 2029 at a compound annual growth rate (CAGR) of 27.6%. The growth in the forecast period can be attributed to increasing sophistication of fraud schemes, integration of predictive analytics, regulatory evolution, global pandemic impact, enhanced patient identity verification. Major trends in the forecast period include adoption of cloud-based analytics, user-friendly interfaces, automation in fraud investigations, real-time fraud detection, behavioral analytics.
A significant rise in fraudulent activities within the healthcare sector is driving the growth of the healthcare fraud analytics market. Fraud can be perpetrated by medical providers, patients, and third parties who intentionally deceive the healthcare system to gain unlawful benefits through deception or misrepresentation. Common fraudulent practices include kickbacks, improper billing, billing for services not rendered, and other deceptive activities. For instance, in December 2023, the U.S. Department of Health and Human Services (HHS) reported that healthcare fraud investigations resulted in recoveries totaling over $1.72 billion, with about $1.2 billion being returned to the Medicare Trust Funds. Furthermore, the Department of Justice (DOJ) noted that in fiscal year 2023, settlements and judgments under the False Claims Act exceeded $2.68 billion, highlighting a robust enforcement response to fraudulent practices. These statistics underscore the substantial financial impact of healthcare fraud, which is estimated to cost the nation billions annually, with some estimates suggesting losses could reach as high as 10% of annual healthcare expenditures. Thus, the increasing prevalence of fraudulent activities in healthcare is significantly contributing to the growth of the healthcare fraud analytics market.
Increased healthcare expenditure is expected to propel the growth of the healthcare fraud analytics market. Healthcare expenditure refers to the total amount of resources, including financial and non-financial, spent on healthcare services and related activities within a specific period of time. Healthcare organizations and payers are investing in advanced fraud analytics solutions to protect their financial resources. For instance, in October 2022, according to the Willis Towers Watson Public Limited Company, a UK-based risk management, insurance brokerage, and advisory company, the healthcare benefit cost increased from 8. 2% in 2021 to 8. 8% in 2022 and is expected to grow again in 2023 to a high global average of 10%. Therefore, increased healthcare expenditure is driving the growth of the healthcare fraud analytics market.
Key players in the healthcare fraud analytics market are concentrating on investments to enhance their presence in the industry. The growing technological advancements in healthcare fraud analytics reflect an increasing allocation of financial resources towards sophisticated analytical tools and technologies designed to detect and prevent fraudulent activities within the sector. For example, in August 2024, MediBuddy, a digital healthcare company based in India, launched an innovative AI-powered fraud detection system called Sherlock. This system aims to combat healthcare fraud, particularly in the area of medical reimbursement claims. The advanced platform employs state-of-the-art artificial intelligence (AI) and machine learning (ML) technologies to identify and prevent fraudulent activities in real-time, thereby improving the integrity of the healthcare system.
Major players in the healthcare fraud analytics market are focusing on strategic partnership to protect customers. Strategic partnerships refer to a process in which companies leverage each other's strengths and resources to achieve mutual benefits and success. For instance, in May 2023, Mastercard, a New-York-based credit card company, partnered with HealthLock, a US-based comapny that provides medical fraud and overbilling protection solution. The collaboration between Mastercard and HealthLock will help safeguard consumers from healthcare fraud and billing errors by delivering a no-fee, core HealthLock breach alert and fraud remediation solution. This service will assist clients in detecting and correcting any fraudulent activity or billing problems on their healthcare bills.
In August 2024, Experian, an Ireland-based business services firm, acquired NeuroID for an undisclosed amount. This acquisition is intended to bolster Experian's identity verification and fraud prevention capabilities by incorporating NeuroID's behavioral analytics technology. This integration will provide deeper insights into consumer behavior and enhance the detection of fraudulent activities across digital interactions. NeuroID is a US-based software company specializing in healthcare fraud analytics.
Major companies operating in the healthcare fraud analytics market include International Business Machines Corporation, Optum Inc., Statistical Analysis Software Institute Inc., Change Healthcare, EXL Service Holdings Inc., Cotiviti Inc., DXC Technology Company, Wipro Limited, Conduent Incorporated, HCL Technologies Limited, Qlarant Inc., LEXIS-NEXIS Group, Healthcare Fraud Shield, FraudLens Inc., HMS Holding Corp., Codoxo, H20. ai, Pondera Solutions Inc., Friss International B. V., MultiPlan Inc., FraudScope, Osp Labs Private Limited, Fair Isaac Corporation, Relx Group PLC.
North America was the largest region in the healthcare fraud analytics market in 2024. North America is expected to be the fastest-growing region in the forecast period. The regions covered in the healthcare fraud analytics market report are Asia-Pacific, Western Europe, Eastern Europe, North America, South America, Middle East, Africa. The countries covered in the healthcare fraud analytics market report are Australia, Brazil, China, France, Germany, India, Indonesia, Japan, Russia, South Korea, UK, USA, Italy, Canada, Spain.
Healthcare fraud analytics refers to on-premise and on-demand analytical solutions that assist in identifying issues such as duplication/repetition of claims and errors in claim healthcare operations and applications. Healthcare fraud analytics aims to help healthcare companies to audit their accounts and find out fraudulent activities in various transactions. It identifies frauds related to billings, claims, prepayment, post payments, and payment integrity.
The main type of solutions in healthcare fraud analytics are descriptive analytics, predictive analytics, prescriptive analytics. Descriptive analytics is a process of using current and historical data to identify trends and relationships. Healthcare fraud analytic solutions are deployed on-premise and on-demand, and they are widely used for insurance claims review, postpayment review, prepayment review, pharmacy billing misuse, payment integrity, other applications. Healthcare fraud analytics are used by public & government agencies, private insurance payers, third-party service providers.
The healthcare fraud analytics market research report is one of a series of new reports that provides healthcare fraud analytics market statistics, including healthcare fraud analytics industry global market size, regional shares, competitors with a healthcare fraud analytics market share, detailed healthcare fraud analytics market segments, market trends and opportunities, and any further data you may need to thrive in the healthcare fraud analytics industry. This healthcare fraud analytics market research report delivers a complete perspective of everything you need, with an in-depth analysis of the current and future scenarios of the industry.
The healthcare fraud analytics market includes revenues earned by entities by providing services such as fraud detection, predictive analytics, and Medicaid. The market value includes the value of related goods sold by the service provider or included within the service offering. Only goods and services traded between entities or sold to end consumers are included.
The market value is defined as the revenues that enterprises gain from the sale of goods and/or services within the specified market and geography through sales, grants, or donations in terms of the currency (in USD, unless otherwise specified).
The revenues for a specified geography are consumption values that are revenues generated by organizations in the specified geography within the market, irrespective of where they are produced. It does not include revenues from resales along the supply chain, either further along the supply chain or as part of other products.
This product will be delivered within 3-5 business days.
Table of Contents
Executive Summary
Healthcare Fraud Analytics Global Market Report 2025 provides strategists, marketers and senior management with the critical information they need to assess the market.This report focuses on healthcare fraud analytics market which is experiencing strong growth. The report gives a guide to the trends which will be shaping the market over the next ten years and beyond.
Reasons to Purchase:
- Gain a truly global perspective with the most comprehensive report available on this market covering 15 geographies.
- Assess the impact of key macro factors such as conflict, pandemic and recovery, inflation and interest rate environment and the 2nd Trump presidency.
- Create regional and country strategies on the basis of local data and analysis.
- Identify growth segments for investment.
- Outperform competitors using forecast data and the drivers and trends shaping the market.
- Understand customers based on the latest market shares.
- Benchmark performance against key competitors.
- Suitable for supporting your internal and external presentations with reliable high quality data and analysis
- Report will be updated with the latest data and delivered to you along with an Excel data sheet for easy data extraction and analysis.
- All data from the report will also be delivered in an excel dashboard format.
Description
Where is the largest and fastest growing market for healthcare fraud analytics? How does the market relate to the overall economy, demography and other similar markets? What forces will shape the market going forward? The healthcare fraud analytics market global report answers all these questions and many more.The report covers market characteristics, size and growth, segmentation, regional and country breakdowns, competitive landscape, market shares, trends and strategies for this market. It traces the market’s historic and forecast market growth by geography.
- The market characteristics section of the report defines and explains the market.
- The market size section gives the market size ($b) Covering both the historic growth of the market, and forecasting its development.
- The forecasts are made after considering the major factors currently impacting the market. These include:
- The forecasts are made after considering the major factors currently impacting the market. These include the Russia-Ukraine war, rising inflation, higher interest rates, and the legacy of the COVID-19 pandemic.
- Market segmentations break down the market into sub markets.
- The regional and country breakdowns section gives an analysis of the market in each geography and the size of the market by geography and compares their historic and forecast growth. It covers the growth trajectory of COVID-19 for all regions, key developed countries and major emerging markets.
- The competitive landscape chapter gives a description of the competitive nature of the market, market shares, and a description of the leading companies. Key financial deals which have shaped the market in recent years are identified.
- The trends and strategies section analyses the shape of the market as it emerges from the crisis and suggests how companies can grow as the market recovers.
Scope
Markets Covered:
1) By Solution Type: Descriptive Analytics; Predictive Analytics; Prescriptive Analytics2) By Delivery Model: on-Premise; on-Demand
3) By Application: Insurance Claims Review; Postpayment Review; Prepayment Review; Pharmacy Billing Misuse; Payment Integrity; Other Applications
Subsegments:
1) By Descriptive Analytics: Data Aggregation; Reporting Tools; Visualization Techniques2) By Predictive Analytics: Risk Assessment Models; Trend analysis; Anomaly Detection
3) By Prescriptive Analytics: Recommendation Engines; Simulation Models; Resource Allocation Tools
Key Companies Mentioned: International Business Machines Corporation; Optum Inc.; Statistical Analysis Software Institute Inc.; Change Healthcare; EXL Service Holdings Inc.
Countries: Australia; Brazil; China; France; Germany; India; Indonesia; Japan; Russia; South Korea; UK; USA; Canada; Italy; Spain
Regions: Asia-Pacific; Western Europe; Eastern Europe; North America; South America; Middle East; Africa
Time Series: Five years historic and ten years forecast.
Data: Ratios of market size and growth to related markets, GDP proportions, expenditure per capita.
Data Segmentation: Country and regional historic and forecast data, market share of competitors, market segments.
Sourcing and Referencing: Data and analysis throughout the report is sourced using end notes.
Delivery Format: PDF, Word and Excel Data Dashboard.
Companies Mentioned
Some of the major companies featured in this Healthcare Fraud Analytics market report include:- International Business Machines Corporation
- Optum Inc.
- Statistical Analysis Software Institute Inc.
- Change Healthcare
- EXL Service Holdings Inc.
- Cotiviti Inc.
- DXC Technology Company
- Wipro Limited
- Conduent Incorporated
- HCL Technologies Limited
- Qlarant Inc.
- LEXIS-NEXIS Group
- Healthcare Fraud Shield
- FraudLens Inc.
- HMS Holding Corp.
- Codoxo
- H20. ai
- Pondera Solutions Inc.
- Friss International B. V.
- MultiPlan Inc.
- FraudScope
- Osp Labs Private Limited
- Fair Isaac Corporation
- Relx Group PLC
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 200 |
| Published | February 2025 |
| Forecast Period | 2025 - 2029 |
| Estimated Market Value ( USD | $ 4.67 Billion |
| Forecasted Market Value ( USD | $ 12.38 Billion |
| Compound Annual Growth Rate | 27.6% |
| Regions Covered | Global |
| No. of Companies Mentioned | 25 |