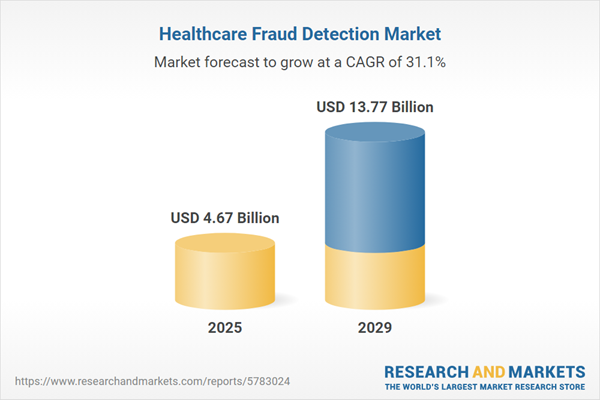
The healthcare fraud detection market size is expected to see exponential growth in the next few years. It will grow to $13.77 billion in 2029 at a compound annual growth rate (CAGR) of 31.1%. The growth in the forecast period can be attributed to regulatory changes, increasing digitalization, sophistication of fraud schemes, focus on insurance fraud, data security enhancement. Major trends in the forecast period include advanced technology integration, real-time monitoring, behavioral analytics, blockchain for security, patient identity verification.
The increasing incidence of fraudulent activities in the healthcare sector is anticipated to drive the growth of the healthcare fraud detection market. Fraudulent events in healthcare involve the intentional misrepresentation of patient information and insurance details to gain unfair or illegal benefits or to deny a user their legal rights. For example, a report from a UK-based financial organization indicated that in 2022, there were 207,372 cases of Authorized Push Payment (APP) fraud, resulting in total losses of £485.2 million, which represents a 17% decrease compared to 2021. Consequently, the rise in fraudulent occurrences within the healthcare industry is expected to propel the demand for healthcare fraud detection solutions.
The ongoing digital transformation in healthcare is projected to significantly boost the growth of the healthcare fraud detection market in the future. As healthcare processes become increasingly digitized, the rising volume and complexity of electronic data, combined with the integration of advanced technologies such as artificial intelligence and machine learning, create an environment conducive to potential fraudulent activities. Digital transformation facilitates real-time monitoring, streamlined data sharing, and improved security measures, enabling fraud detection systems to swiftly identify irregularities. Moreover, the implementation of electronic health records, remote healthcare services, and electronic claims processing requires robust fraud detection solutions to protect against unauthorized access and fraudulent activities. For instance, a report published by gov.UK in February 2024 noted that in 2022, the digital sector contributed approximately $171.25 million to the UK economy, representing 7.2% of the total UK gross value added (GVA), which is a slight increase from 7.1% in 2021. Thus, the rise of digital transformation in healthcare is driving the expansion of the healthcare fraud detection market.
The adoption of advanced analytics tools emerges as a significant trend gaining traction within the healthcare fraud detection landscape. Key industry players are channeling efforts into crafting innovative technologies to maintain their foothold in the healthcare fraud detection sphere. For instance, in January 2022, Premier, Inc., a US-based healthcare technology company, introduced 'INSights' built upon PINC AITM technology. INSights stand as a vendor-neutral analytics platform harnessing risk-adjusted, standardized, and cleansed healthcare data from PINC AITM. Tailored for healthcare providers, INSights aim to alleviate the burden associated with data preparation and analytics development, enabling rapid improvements in clinical, quality, and financial outcomes.
Leading companies within the healthcare fraud detection arena are innovating new insurance fraud detection solutions to gain a competitive edge. For example, in June 2023, Verisk Analytics, Inc., a US-based analytics company, collaborated with Kyndryl Holdings, Inc. to introduce an advanced technology suite targeting insurance fraud prevention in Israel's compulsory insurance market. Leveraging Kyndryl's robust computing resources and Verisk's domain expertise, this solution fortified the anti-fraud engine for real-time monitoring of auto claims concerning bodily injury. Supported by round-the-clock managed services and advanced analytics, the system verified applicant details against databases and government sources, facilitating comprehensive data investigations for insurance claim adjusters. This collaboration aimed to streamline claims processes, detect potential fraud, and meet evolving consumer expectations in the digitized insurance landscape.
In October 2022, Levio Conseils Inc., a Canadian digital consulting firm specializing in information technology and organizational management, acquired Indellient for an undisclosed amount. This acquisition is intended to help Levio Conseils Inc. expand its service offerings, strengthen its market presence, and leverage new technologies to enhance client services. Indellient, also based in Canada, specializes in software development, cloud solutions, and digital transformation services.
Major companies operating in the healthcare fraud detection market are International Business Machines Corporation, Cotiviti Inc., Fair Isaac Corporation, SAS Institute Inc., CGI Inc., DXC Technology Company, RELX Group PLC, EXL Service Holdings Inc., HCL Technologies Limited, UnitedHealth Group Incorporated, Conduent Incorporated, Change Healthcare LLC, OSP Labs LLC, Codoxo Inc., Wipro Limited, Qlarant Inc., Northrop Grumman Corporation, LexisNexis Risk Solutions Group, Healthcare Fraud Shield LLC, Sharecare Inc., FraudLens Inc., HMS Holdings Corp., H2O.ai Inc., Pondera Solutions Inc., FRISS B.V., MultiPlan Corporation, FraudScope Inc., McKesson Corporation, FraudGuard LLC, FraudCracker LLC.
North America was the largest region in the healthcare fraud detection market in 2024. The regions covered in the healthcare fraud detection market report are Asia-Pacific, Western Europe, Eastern Europe, North America, South America, Middle East, Africa. The countries covered in the healthcare fraud detection market report are Australia, Brazil, China, France, Germany, India, Indonesia, Japan, Russia, South Korea, UK, USA, Canada, Italy, Spain.
Healthcare fraud detection involves measures taken to prevent individuals from acquiring patient data or assets through deceptive means. This encompasses auditing accounts and conducting investigative procedures to ensure transparency, accountability, and risk assessment. Its aim is to identify, prevent, and manage potential instances of fraud, waste, or abuse, thereby reducing the compromise of sensitive patient information like medical records.
The primary categories of healthcare fraud detection comprise descriptive, predictive, and prescriptive analytics. Descriptive analytics, leveraging historical and current data, unearth patterns and connections to flag suspicious activities. These analytics support the management of medical imaging, clinical data, and outcomes. There are two delivery models such as on-premise and on-demand, utilizing services and software components. These methods find application in insurance claim reviews and payment integrity, serving healthcare payers, government bodies, and other stakeholders.
The healthcare fraud detection market research report is one of a series of new reports that provides healthcare fraud detection market statistics, including healthcare fraud detection industry global market size, regional shares, competitors with an healthcare fraud detection market share, detailed healthcare fraud detection market segments, market trends and opportunities, and any further data you may need to thrive in the healthcare fraud detection industry. This healthcare fraud detection market research report delivers a complete perspective of everything you need, with an in-depth analysis of the current and future scenario of the industry.
The health fraud detection market includes revenues earned by entities by tracking secondary data, providing technology specialist. The market value includes the value of related goods sold by the service provider or included within the service offering. Only goods and services traded between entities or sold to end consumers are included.
The market value is defined as the revenues that enterprises gain from the sale of goods and/or services within the specified market and geography through sales, grants, or donations in terms of the currency (in USD, unless otherwise specified).
The revenues for a specified geography are consumption values that are revenues generated by organizations in the specified geography within the market, irrespective of where they are produced. It does not include revenues from resales along the supply chain, either further along the supply chain or as part of other products.
This product will be delivered within 3-5 business days.
Table of Contents
Executive Summary
Healthcare Fraud Detection Global Market Report 2025 provides strategists, marketers and senior management with the critical information they need to assess the market.This report focuses on healthcare fraud detection market which is experiencing strong growth. The report gives a guide to the trends which will be shaping the market over the next ten years and beyond.
Reasons to Purchase:
- Gain a truly global perspective with the most comprehensive report available on this market covering 15 geographies.
- Assess the impact of key macro factors such as conflict, pandemic and recovery, inflation and interest rate environment and the 2nd Trump presidency.
- Create regional and country strategies on the basis of local data and analysis.
- Identify growth segments for investment.
- Outperform competitors using forecast data and the drivers and trends shaping the market.
- Understand customers based on the latest market shares.
- Benchmark performance against key competitors.
- Suitable for supporting your internal and external presentations with reliable high quality data and analysis
- Report will be updated with the latest data and delivered to you along with an Excel data sheet for easy data extraction and analysis.
- All data from the report will also be delivered in an excel dashboard format.
Description
Where is the largest and fastest growing market for healthcare fraud detection? How does the market relate to the overall economy, demography and other similar markets? What forces will shape the market going forward? The healthcare fraud detection market global report answers all these questions and many more.The report covers market characteristics, size and growth, segmentation, regional and country breakdowns, competitive landscape, market shares, trends and strategies for this market. It traces the market’s historic and forecast market growth by geography.
- The market characteristics section of the report defines and explains the market.
- The market size section gives the market size ($b) covering both the historic growth of the market, and forecasting its development.
- The forecasts are made after considering the major factors currently impacting the market. These include:
- The forecasts are made after considering the major factors currently impacting the market. These include the Russia-Ukraine war, rising inflation, higher interest rates, and the legacy of the COVID-19 pandemic.
- Market segmentations break down the market into sub markets.
- The regional and country breakdowns section gives an analysis of the market in each geography and the size of the market by geography and compares their historic and forecast growth. It covers the growth trajectory of COVID-19 for all regions, key developed countries and major emerging markets.
- The competitive landscape chapter gives a description of the competitive nature of the market, market shares, and a description of the leading companies. Key financial deals which have shaped the market in recent years are identified.
- The trends and strategies section analyses the shape of the market as it emerges from the crisis and suggests how companies can grow as the market recovers.
Scope
Markets Covered:
1) by Type: Descriptive Analytics; Predictive Analytics; Prescriptive Analytics2) by Model: on-Premise Delivery; on-Demand Delivery
3) by Component: Services; Software
4) by Application: Insurance Claims Review; Payment Integrity
5) by End User: Healthcare Payers; Government Agencies; Other End-Users
Subsegments:
1) by Descriptive Analytics: Data Mining; Reporting Tools; Historical Data Analysis2) by Predictive Analytics: Risk Scoring Models; Machine Learning Algorithms; Trend Analysis
3) by Prescriptive Analytics: Decision Support Systems; Optimization Algorithms; Scenario Analysis and Simulations
Key Companies Mentioned: International Business Machines Corporation; Cotiviti Inc.; Fair Isaac Corporation; SAS Institute Inc.; CGI Inc.
Countries: Australia; Brazil; China; France; Germany; India; Indonesia; Japan; Russia; South Korea; UK; USA; Canada; Italy; Spain
Regions: Asia-Pacific; Western Europe; Eastern Europe; North America; South America; Middle East; Africa
Time Series: Five years historic and ten years forecast.
Data: Ratios of market size and growth to related markets, GDP proportions, expenditure per capita.
Data Segmentation: Country and regional historic and forecast data, market share of competitors, market segments.
Sourcing and Referencing: Data and analysis throughout the report is sourced using end notes.
Delivery Format: PDF, Word and Excel Data Dashboard.
Companies Mentioned
Some of the major companies featured in this Healthcare Fraud Detection market report include:- International Business Machines Corporation
- Cotiviti Inc.
- Fair Isaac Corporation
- SAS Institute Inc.
- CGI Inc.
- DXC Technology Company
- RELX Group PLC
- EXL Service Holdings Inc.
- HCL Technologies Limited
- UnitedHealth Group Incorporated
- Conduent Incorporated
- Change Healthcare LLC
- OSP Labs LLC
- Codoxo Inc.
- Wipro Limited
- Qlarant Inc.
- Northrop Grumman Corporation
- LexisNexis Risk Solutions Group
- Healthcare Fraud Shield LLC
- Sharecare Inc.
- FraudLens Inc.
- HMS Holdings Corp.
- H2O.ai Inc.
- Pondera Solutions Inc.
- FRISS B.V.
- MultiPlan Corporation
- FraudScope Inc.
- McKesson Corporation
- FraudGuard LLC
- FraudCracker LLC
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 200 |
| Published | February 2025 |
| Forecast Period | 2025 - 2029 |
| Estimated Market Value ( USD | $ 4.67 Billion |
| Forecasted Market Value ( USD | $ 13.77 Billion |
| Compound Annual Growth Rate | 31.1% |
| Regions Covered | Global |
| No. of Companies Mentioned | 31 |