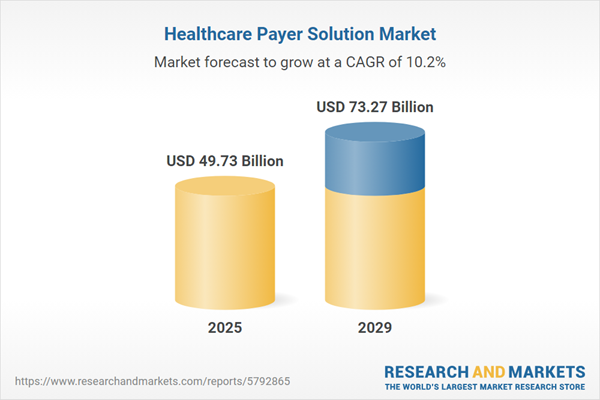
The healthcare payer solution market size is expected to see rapid growth in the next few years. It will grow to $73.27 billion in 2029 at a compound annual growth rate (CAGR) of 10.2%. The growth in the forecast period can be attributed to shift towards patient-centric care, rise in telemedicine and remote care, increased emphasis on data security, value-based payment models. Major trends in the forecast period include financial transparency and cost management, risk stratification and population health management, data interoperability and exchange, rise of value-based care models, integration of AI and predictive analytics.
The anticipated increase in insurance enrolments is poised to drive the growth of the healthcare payer solutions market. Insurance enrolment is the process by which a qualified applicant registers with the insurance provider and becomes a member of the plan. In the insurance market, healthcare payer solutions offer robust enterprise core administration and claim management platform solutions, fostering expansion, innovation, and cost savings for payer organizations across various business lines. For example, as reported by the Centers for Medicare & Medicaid Services in the USA, more than 13.6 million Americans enrolled in health insurance coverage for 2022 through HealthCare.gov and State-based Marketplaces, constituting 92% of those who registered for plans by December 15, 2021. Consequently, the increasing insurance enrolments are fueling the demand for the healthcare payer solutions market.
The upward trend in the aging population is expected to drive the growth of healthcare payer solutions in the future. An aging population denotes a demographic shift marked by a rising proportion of elderly individuals within a society over time. Healthcare payer solutions play a crucial role in helping the aging population streamline insurance processes, enhance patient care coordination, and improve financial management, addressing the specific needs and complexities associated with elderly healthcare. For example, the World Health Organization projected in October 2022 that by 2030, one out of every six individuals globally would be 60 years old or older. The proportion of the population aged 60 and over is expected to increase from 1 billion in 2020 to 1.4 billion during this period. Additionally, by 2050, the global population of individuals aged 60 and older is projected to double, reaching 2.1 billion. Therefore, the rising aging population is a driving force for the healthcare payer solutions market.
Product innovations emerge as a significant trend gaining traction in the healthcare payer solutions market. Major companies in this sector are dedicated to developing innovative solutions to fortify their business positions. For instance, in March 2022, IMAT Solutions, a US-based provider of innovative, real-time healthcare data management, and population health reporting solutions, introduced a new product addressing the gathering, aggregation, dissemination, and reporting of healthcare data. The new technologies and services from IMAT Solutions enable payers, statewide organizations, and Health Information Exchanges (HIEs) to leverage clustering and Software as a Service (SaaS)-based solutions, in addition to the company's new National Committee for Quality Assurance (NCQA) Data Aggregator Validation (DAV) designation.
Major companies operating in the healthcare payer solutions market are focusing on developing advanced solutions such as Payer Exchange to handle the escalating volumes of medical records and clinical data. Payer Exchange is a technological solution designed to facilitate clinical data exchange between healthcare providers and payers. For example, in June 2023, MRO Corp, a US-based clinical data exchange company, launched a Payer Exchange solution. This technology digitizes and automates the patient information request and fulfillment process, reducing manual burdens for hospital staff and improving workflows. Payer Exchange addresses the growing demand from payers for high-quality and timely clinical data, providing a secure, electronic connection for efficient communication between providers and payers. The solution emphasizes patient privacy, data quality, and risk adjustment premium accuracy.
In September 2022, Zelis, a US-based healthcare and financial technology growth company, acquired Payer Compass for an undisclosed amount. Through this acquisition, Zelis and Payer Compass aim to collaborate as a single organization to advance claims management solutions and make a substantial impact on the complexity and rising costs of healthcare. Payer Compass is a US-based provider in the healthcare industry offering reimbursement and claims pricing, administration, and processing solutions.
Major companies operating in the healthcare payer solution market include Cognizant Technical Solutions, Concentrix Corporation, Accenture plc, HCL Technologies Ltd., Xerox Corporation, UnitedHealth Group Inc., McKesson Corporation, HMS Holdings Corp., International Business Machines Corporation, Change Healthcare Inc., Wipro Limited, Infosys Limited, Tata Consultancy Services Limited, NTT Data Corporation, Genpact Limited, Mphasis Limited, Firstsource Solutions Limited, WNS Limited, IQVIA Inc., Omega Healthcare, R RCM Inc., Conduent Inc., EXL Service Holdings Inc., Cotiviti Holdings Inc., Cerner Corporation, Allscripts Healthcare Solutions Inc., Epic Systems Corporation, Athenahealth Inc., NextGen Healthcare Inc., eClinicalWorks LLC.
North America was the largest region in the healthcare payer solution market in 2024. The regions covered in the healthcare payer solution market report are Asia-Pacific, Western Europe, Eastern Europe, North America, South America, Middle East, Africa. The countries covered in the healthcare payer solution market report are Australia, Brazil, China, France, Germany, India, Indonesia, Japan, Russia, South Korea, UK, USA, Canada, Italy, Spain.
Healthcare payer solutions refer to tools and services designed to assist healthcare insurers, both public and private, as well as members in managing various aspects such as claims, member engagement, audits, medical records, and customer relations. These solutions play a crucial role in enhancing the overall performance of the healthcare system by improving care quality, reducing costs, increasing patient satisfaction, enhancing provider effectiveness, and leveraging unique competencies.
The main services offered by healthcare payer solutions include business process outsourcing services, information technology outsourcing services, and knowledge process outsourcing services. Business process outsourcing involves the transfer of one or more intensive business processes to a third party, who then takes responsibility for owning, administering, and maintaining the specified processes based on predetermined and quantifiable performance goals. Various applications within healthcare payer solutions include pharmacy audit and analysis systems, claims management services, fraud management services, computer-assisted coding (CAC) systems, member eligibility management services, provider network management services, payment management services, customer relationship management services, medical document management services, and general ledger and payroll management. These applications are utilized by both private and public provider end-users.
The healthcare payer solutions market research report is one of a series of new reports that provides healthcare payer solutions market statistics, including healthcare payer solutions industry global market size, regional shares, competitors with healthcare payer solutions market share, detailed healthcare payer solutions market segments, market trends, and opportunities, and any further data you may need to thrive in the healthcare payer solutions industry. This healthcare payer solutions market research report delivers a complete perspective of everything you need, with an in-depth analysis of the current and future scenarios of the industry.
The healthcare payer solution market includes revenues earned by entities by providing product assessments, health plan member engagement, and payer analytics. The market value includes the value of related goods sold by the service provider or included within the service offering. Only goods and services traded between entities or sold to end consumers are included.
The market value is defined as the revenues that enterprises gain from the sale of goods and/or services within the specified market and geography through sales, grants, or donations in terms of the currency (in USD, unless otherwise specified).
The revenues for a specified geography are consumption values that are revenues generated by organizations in the specified geography within the market, irrespective of where they are produced. It does not include revenues from resales along the supply chain, either further along the supply chain or as part of other products.
This product will be delivered within 3-5 business days.
Table of Contents
Executive Summary
Healthcare Payer Solution Global Market Report 2025 provides strategists, marketers and senior management with the critical information they need to assess the market.This report focuses on healthcare payer solution market which is experiencing strong growth. The report gives a guide to the trends which will be shaping the market over the next ten years and beyond.
Reasons to Purchase:
- Gain a truly global perspective with the most comprehensive report available on this market covering 15 geographies.
- Assess the impact of key macro factors such as conflict, pandemic and recovery, inflation and interest rate environment and the 2nd Trump presidency.
- Create regional and country strategies on the basis of local data and analysis.
- Identify growth segments for investment.
- Outperform competitors using forecast data and the drivers and trends shaping the market.
- Understand customers based on the latest market shares.
- Benchmark performance against key competitors.
- Suitable for supporting your internal and external presentations with reliable high quality data and analysis
- Report will be updated with the latest data and delivered to you along with an Excel data sheet for easy data extraction and analysis.
- All data from the report will also be delivered in an excel dashboard format.
Description
Where is the largest and fastest growing market for healthcare payer solution ? How does the market relate to the overall economy, demography and other similar markets? What forces will shape the market going forward? The healthcare payer solution market global report answers all these questions and many more.The report covers market characteristics, size and growth, segmentation, regional and country breakdowns, competitive landscape, market shares, trends and strategies for this market. It traces the market’s historic and forecast market growth by geography.
- the market characteristics section of the report defines and explains the market.
- the market size section gives the market size ($b) covering both the historic growth of the market, and forecasting its development.
- the forecasts are made after considering the major factors currently impacting the market. These include:
- the forecasts are made after considering the major factors currently impacting the market. These include the Russia-Ukraine war, rising inflation, higher interest rates, and the legacy of the COVID-19 pandemic.
- Market segmentations break down the market into sub markets.
- the regional and country breakdowns section gives an analysis of the market in each geography and the size of the market by geography and compares their historic and forecast growth. It covers the growth trajectory of COVID-19 for all regions, key developed countries and major emerging markets.
- the competitive landscape chapter gives a description of the competitive nature of the market, market shares, and a description of the leading companies. Key financial deals which have shaped the market in recent years are identified.
- the trends and strategies section analyses the shape of the market as it emerges from the crisis and suggests how companies can grow as the market recovers.
Scope
Markets Covered:
1) by Services: Business Process Outsourcing Services; Information Technology Outsourcing Services; Knowledge Process Outsourcing Services2) by Application: Pharmacy Audit and Analysis Systems; Claims Management Services; Fraud Management Services; Computer-assisted Coding (CAC) Systems; Member Eligibility Management Services; Provider Network Management Services; Payment Management Services; Customer Relationship Management Services; Medical Document Management Services; General Ledger and Payroll Management
3) by End User: Private Provider; Public Provider
Subsegments:
1) by Business Process Outsourcing Services: Claims Processing; Enrollment and Eligibility Verification; Member Services and Support; Provider Network Management; Billing and Payment Processing; Data Management and Analytics2) by Information Technology Outsourcing Services: Application Development and Maintenance; IT Infrastructure Management; Data Security and Compliance Solutions; Cloud Services; Health Information Exchange Solutions; Software As a Service (SaaS) Solutions
3) by Knowledge Process Outsourcing Services: Clinical Data Management; Healthcare Analytics; Market Research and Intelligence; Medical Coding and Billing Services; Regulatory Compliance Services; Health Outcomes Research
Key Companies Mentioned: Cognizant Technical Solutions; Concentrix Corporation; Accenture plc; HCL Technologies Ltd.; Xerox Corporation
Countries: Australia; Brazil; China; France; Germany; India; Indonesia; Japan; Russia; South Korea; UK; USA; Canada; Italy; Spain
Regions: Asia-Pacific; Western Europe; Eastern Europe; North America; South America; Middle East; Africa
Time Series: Five years historic and ten years forecast.
Data: Ratios of market size and growth to related markets, GDP proportions, expenditure per capita.
Data Segmentation: Country and regional historic and forecast data, market share of competitors, market segments.
Sourcing and Referencing: Data and analysis throughout the report is sourced using end notes.
Delivery Format: PDF, Word and Excel Data Dashboard.
Companies Mentioned
Some of the major companies featured in this Healthcare Payer Solution market report include:- Cognizant Technical Solutions
- Concentrix Corporation
- Accenture plc
- HCL Technologies Ltd.
- Xerox Corporation
- UnitedHealth Group Inc.
- McKesson Corporation
- HMS Holdings Corp.
- International Business Machines Corporation
- Change Healthcare Inc.
- Wipro Limited
- Infosys Limited
- Tata Consultancy Services Limited
- NTT Data Corporation
- Genpact Limited
- Mphasis Limited
- Firstsource Solutions Limited
- WNS Limited
- IQVIA Inc.
- Omega Healthcare
- R RCM Inc.
- Conduent Inc.
- EXL Service Holdings Inc.
- Cotiviti Holdings Inc.
- Cerner Corporation
- Allscripts Healthcare Solutions Inc.
- Epic Systems Corporation
- Athenahealth Inc.
- NextGen Healthcare Inc.
- eClinicalWorks LLC
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 200 |
| Published | February 2025 |
| Forecast Period | 2025 - 2029 |
| Estimated Market Value ( USD | $ 49.73 Billion |
| Forecasted Market Value ( USD | $ 73.27 Billion |
| Compound Annual Growth Rate | 10.2% |
| Regions Covered | Global |
| No. of Companies Mentioned | 31 |