Speak directly to the analyst to clarify any post sales queries you may have.
MARKET TRENDS AND DRIVERS
Increasing Healthcare Fraudulent Activities
Healthcare fraud has been an ongoing problem in the healthcare industry for a long time. The increase in healthcare costs, the rise in technological advances, and a greater reliance on electronic data have all contributed to an increase in healthcare fraud. The healthcare fraud analytics market helps combat this issue by identifying fraudulent activities and helping organizations take proactive measures to prevent future fraud. Healthcare fraud analytics uses various analytic techniques to analyze large datasets and detect suspicious behavior patterns. These techniques can detect billing and coding errors, improper payments, and other forms of fraud. Healthcare fraud analytics also helps organizations identify trends in healthcare fraud and proactively address areas of risk. The increasing prevalence of healthcare fraud is driving the demand for healthcare fraud analytics solutions. Organizations increasingly invest in healthcare fraud analytics solutions to detect and prevent fraudulent activities and protect their financial and reputational interests.The Increasing Number of Patients Benefiting From Healthcare Insurance
Healthcare fraud analytics uses data analytics and artificial intelligence to detect fraud and patterns in healthcare claims and other activities related to healthcare fraud. With the increasing number of patients receiving healthcare insurance, the potential amount of fraud increases, making it essential to have a reliable fraud detection system. The healthcare fraud analytics market helps to detect fraudulent activities such as billing for services not rendered and incorrect coding. With the increasing number of healthcare policies, fraudulent activities also increase, making identifying and preventing them difficult. Healthcare fraud analytics helps to identify these activities quickly and accurately, thus reducing the risk of fraud.The Increasing Number of Pharmacy Claims-Related Frauds
With the growth of the healthcare industry, fraud & abuse have become increasingly serious problems. Fraudsters are taking advantage of the complexity of the healthcare system and the lack of oversight to commit fraud. As a result, healthcare organizations are facing increasing pressure to protect their finances from fraudulent activities. The healthcare fraud analytics market is growing as healthcare organizations begin recognizing the need for advanced analytics solutions to detect and prevent fraud. Healthcare analytics solutions are used to identify suspicious transactions and activities that could indicate fraudulent behavior. These solutions help detect and prevent fraud by providing insights into fraud patterns, allowing organizations to take corrective action.Investment in ICT
Investment in ICT is a new opportunity for the healthcare fraud analytics market. ICT solutions such as Artificial Intelligence (AI) and Machine Learning (ML) can be used to detect and prevent fraud in the healthcare industry. By leveraging these technologies, healthcare organizations can develop and deploy predictive analytics models to detect suspicious transactions, identity theft, and other fraudulent activities. This can help organizations reduce the risk of fraud, save money, and improve operational efficiency.Advanced Technologies Offer Greater Potential to Secure Against Fraud
Advanced technologies offer greater potential to secure against fraud, and this is a new opportunity for the healthcare fraud analytics market. With the increasing sophistication of fraud attempts, the need for advanced analytics tools to detect, prevent, and investigate fraud is becoming more important. Advanced analytics tools can help detect and prevent fraud more quickly and efficiently while providing more detailed insights into fraud patterns. This can help healthcare organizations identify potential areas of fraud and take steps to reduce the risk. In addition, advanced analytics can help healthcare organizations detect and investigate fraud more effectively, which can help reduce the financial losses associated with fraudulent activities.AI in Healthcare Fraud Detection
AI in healthcare fraud detection is a new opportunity for the healthcare fraud analytics market. AI can detect and prevent fraud more quickly and accurately than traditional methods, reducing financial and administrative costs. AI can identify patterns in large amounts of data that would be impossible to find using manual methods and identify suspicious behavior that would be difficult to detect using traditional methods. AI can also help organizations identify and address fraud risk areas more quickly, as well as help them develop strategies to prevent future fraud from occurring.SEGMENTATION INSIGHTS
INSIGHTS BY SOLUTION TYPE
The global healthcare fraud analytics market by solution type is segmented into descriptive, predictive, and prescriptive analytics. Descriptive analytics is a form of data analysis that seeks to summarize past events and identify patterns in data. It is a process that involves collecting, organizing, and analyzing data to gain insights that can be used to inform future decisions or strategies. This type of analytics is especially useful for businesses, as it can better understand customer behaviors, sales trends, and performance metrics. Descriptive fraud analytics is the process of analyzing data to detect patterns of fraud and other suspicious activities. It is a type of analytics that helps organizations identify and understand fraud-related activities and detect fraud before it occurs.However, predictive analytics is expected to grow at a CAGR in the global healthcare fraud analytics market during the forecast period. Predictive analytics can also be used to detect trends in healthcare fraud. By analyzing the data from various sources, such as patient records, medical records, and healthcare billing systems, the predictive model can identify patterns of fraud that may not be easily visible.
Segmentation by Solution Type
- Descriptive Analytics
- Predictive Analytics
- Prescriptive Analytics
INSIGHTS BY DELIVERY MODE
The global healthcare fraud analytics market by delivery mode is segmented into on-premises and cloud-based. The on-premises segment dominated the market, accounting for over 52% share in 2022, and is anticipated to retain its dominance during the forecast period. On-premises service allows companies to verify customers and store data on their servers. No third party can access the customers’ data, the service provider, or vendors. This service ensures that their customer onboarding process is secure and the information collected stays safe from criminal activities. Several on-premises benefits also significantly contribute to why healthcare organizations are still hesitant to embrace the cloud. The biggest benefit to on-premises applications is that the IT department has full control over the data stored on them.Segmentation by Delivery Mode
- On-premises
- Cloud-based
INSIGHTS BY APPLICATIONS
The medical provider fraud application segment holds the largest global healthcare fraud analytics market share. Medical provider fraud occurs when a health care provider, such as a doctor, nurse, or therapist, defrauds a medical insurance provider for reimbursement for services that were never provided or for services of a lower quality than what was promised. Both individuals and organizations can perpetrate this type of fraud, which can be difficult to detect due to the complexity of medical billing systems. The most common form of medical provider fraud is billing for never provided services. This may include billing for an office visit that never occurred or for procedures that were not done. This type of fraud can also occur when providers bill for services at a higher rate than what was performed or for more expensive treatments than what was actually given.Segmentation by Application
- Medical Provider Fraud
- Patient Fraud
- Prescription Fraud
- General Healthcare Fraud
INSIGHTS BY END-USER
The global healthcare fraud analytics market by end-user is segmented into public health insurance companies, private health insurance companies, third-party service providers, and other end users. The public health insurance companies segment accounted for a major share in 2022. Public health insurance companies play an integral role in the health and well-being of individuals and the country. By providing financial coverage for medical costs and preventive care, these companies can help keep individuals healthy while reducing healthcare costs. Public health insurance companies have a key role in the global healthcare fraud analytics market. They are responsible for providing healthcare coverage to citizens and are the main funding source for healthcare services. With the rising healthcare costs and the prevalence of fraud and abuse, public health insurance companies must take a proactive approach to combat fraud and abuse. Public health insurance companies can help reduce fraud and abuse by using healthcare fraud analytics tools to identify suspicious activity and detect fraud.Segmentation by End-user
- Public Health Insurance Companies
- Private Health Insurance Companies
- Third-party Service Providers
- Others
GEOGRAPHICAL ANALYSIS
North America accounted for a major share of the global healthcare fraud analytics market in 2022, accounting for nearly 43%. The presence of a large patient population and better adoption of digital healthcare with the latest advancements in artificial intelligence (AI) is the primary factor for its high market share. The presence of key healthcare IT players is another reason for the high uptake of healthcare fraud analytics in North America. The use of healthcare fraud analytics is becoming increasingly common in the United States and Canada. In the United States, the Department of Health and Human Services (HHS) uses healthcare fraud analytics to identify fraud in Medicare and Medicaid.Segmentation by Geography
- North America
- US
- Canada
- Europe
- Germany
- UK
- France
- Italy
- Spain
- APAC
- China
- Japan
- South Korea
- India
- Australia
- Latin America
- Brazil
- Mexico
- Argentina
- Middle East & Africa
- Turkey
- Saudi Arabia
- South Africa
VENDOR LANDSCAPE
The global healthcare fraud analytics market is a rapidly growing industry since fraud and abuse in the healthcare system is an ongoing problem resulting in billions of dollars in losses to insurers and patients. The market is driven by rising healthcare costs, increasing consumer demand for transparency and accountability, and the need to reduce fraud and abuse. The global healthcare fraud analytics market is emerging, with global, regional, and local players recommending a broad range of conventional and latest-generation artificial intelligence (AI) technologies for end-users. The key vendors in the global healthcare fraud analytics market include IBM, LexisNexis Risk Solution, Optum, SAS Institute, Verisk Analytics, and Wipro, based on factors such as digital healthcare platforms, patient management, and clinical advancements. These companies have a broad geographic presence, diverse product portfolios, and a strong focus on product innovation, R&D, and business expansion activities.Key Company Profiles
- IBM
- LexisNexis Risk Solutions
- Optum
- SAS Institute
- Verisk Analytics
- Wipro
Other Prominent Vendors
- Alivia Analytics
- CGI
- Codoxo
- Conduent
- COTIVITI
- FraudLens
- FRISS
- Healthcare Fraud Shield
- Northrop Grumman Corporation
- OSP
- Qlarant
- Qualetics Data Machines
- Sharecare
KEY QUESTIONS ANSWERED:
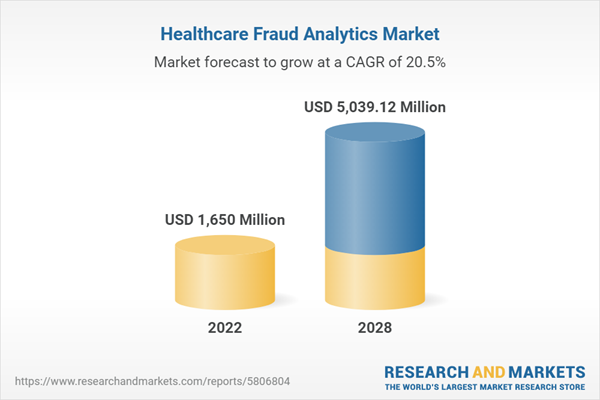
- How big is the global healthcare fraud analytics market?
- What is the growth rate of the healthcare fraud analytics market?
- What are the growing trends in the healthcare fraud analytics market?
- Which region holds the most significant global healthcare fraud analytics market share?
- Who are the key players in the global healthcare fraud analytics market?
Table of Contents
Companies Mentioned
- IBM
- LexisNexis Risk Solutions
- Optum
- SAS Institute
- Verisk Analytics
- Wipro
- Alivia Analytics
- CGI
- Codoxo
- Conduent
- COTIVITI
- FraudLens
- FRISS
- Healthcare Fraud Shield
- Northrop Grumman Corporation
- OSP
- Qlarant
- Qualetics Data Machines
- Sharecare
Methodology
Our research comprises a mix of primary and secondary research. The secondary research sources that are typically referred to include, but are not limited to, company websites, annual reports, financial reports, company pipeline charts, broker reports, investor presentations and SEC filings, journals and conferences, internal proprietary databases, news articles, press releases, and webcasts specific to the companies operating in any given market.
Primary research involves email interactions with the industry participants across major geographies. The participants who typically take part in such a process include, but are not limited to, CEOs, VPs, business development managers, market intelligence managers, and national sales managers. We primarily rely on internal research work and internal databases that we have populated over the years. We cross-verify our secondary research findings with the primary respondents participating in the study.

LOADING...
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 300 |
| Published | May 2023 |
| Forecast Period | 2022 - 2028 |
| Estimated Market Value ( USD | $ 1650 Million |
| Forecasted Market Value ( USD | $ 5039.12 Million |
| Compound Annual Growth Rate | 20.4% |
| Regions Covered | Global |
| No. of Companies Mentioned | 19 |