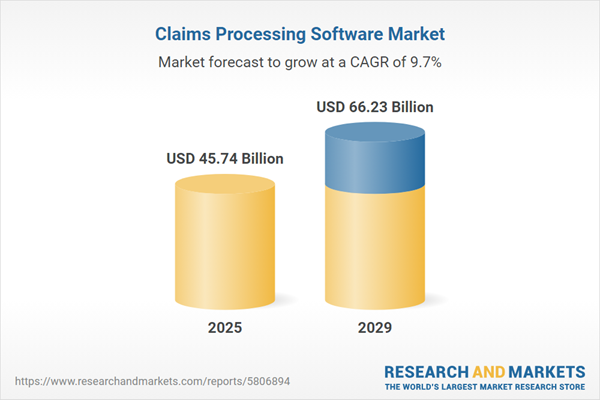
The claims processing software market size is expected to see strong growth in the next few years. It will grow to $66.23 billion in 2029 at a compound annual growth rate (CAGR) of 9.7%. The growth in the forecast period can be attributed to real-time claims processing, mobile claims processing solutions, government initiatives for digital transformation, customer self-service portals, predictive analytics for risk assessment. Major trends in the forecast period include ai and machine learning integration, blockchain adoption for security implementation, integration with IoT devices, telehealth and virtual healthcare, cloud-based claims processing solutions, implementation of robotic process automation.
The growth of the claims processing software market is expected to be propelled by the focus on lowering compliance risk exposure. Compliance risk refers to the potential consequences an organization may face for not adhering to industry laws, regulations, internal policies, or best practices. Claims processing software providers stand to benefit significantly from reducing compliance risk, as it can enhance operational efficiency, cut costs, and bolster their reputation and credibility in the market. Lowering compliance risk also positions them to offer more reliable and efficient solutions to customers, ultimately leading to revenue growth. An example of this is seen in Accenture plc's data from August 2022, revealing that insurers using claims processing software experienced a 38% reduction in fraudulent claims, a 60% reduction in manual intervention, and a 70% reduction in claims settlement time.
The rising healthcare expenditure is anticipated to drive the growth of the claims processing software market in the future. Healthcare expenditure refers to the total amount spent on healthcare goods and services over a specific period, typically a year. It includes various expenses incurred by individuals, private healthcare providers, government agencies, and health insurance companies. As healthcare costs increase, insurers and healthcare providers must manage claims more efficiently to lower administrative costs and enhance patient care. Claims processing software aids in automating workflows, minimizing errors, and improving overall operational efficiency, leading to cost savings for organizations. For instance, in May 2023, a report from the Office for National Statistics, a UK-based government department, revealed that healthcare spending in the UK rose by 5.6% between 2022 and 2023, compared to a growth rate of 0.9% in 2022. The UK's healthcare expenditure reached approximately $317.63 billion (£292 billion) in 2023. Therefore, the increasing healthcare expenditure is propelling the growth of the claims processing software market.
Technological advancements represent a key trend in the claims processing software market. Major players are focusing on innovative technologies to strengthen their market position. Advanced technologies such as chatbots, optical character recognition, advanced analytics, robotic process automation (RPA), and artificial intelligence (AI) have improved the efficiency and accuracy of claims processing. IBM, for instance, launched IBM Robotic Process Automation 21.0.3 in July 2022, showcasing a 200% increase in return on investment (ROI) within the first year of RPA deployment in financial services. RPA and AI are employed for tasks such as collecting customer information, extracting claims data, performing background checks, and more, contributing to the technological advancement in claims processing software.
Major companies in the claims processing software market are strategically focusing on the introduction of advanced solutions to boost their revenues. One such innovative solution is the AI-based claim acceleration suite, a cloud-based automation toolkit leveraging artificial intelligence (AI) and machine learning to streamline health insurance prior authorization and claims processing. For instance, Google Cloud launched an AI-enabled Claims Acceleration Suite in April 2023. This solution transforms unstructured data into structured data, employing the Claims Data Activator to help health plans and providers reduce administrative burdens and costs. The suite enables quicker and more informed decisions, enhancing patient care. Notably, Bupa and Blue Shield of California have implemented this solution to increase efficiency and improve the experiences of patients and providers.
In October 2022, TPG Inc., a prominent US-based private equity firm, acquired Change Healthcare's healthcare claims analytics and payment accuracy software solution, ClaimsXten, for $2.2 billion. This acquisition positions TPG Inc. to expand its capabilities in the healthcare claims processing domain, leading to increased efficiency, enhanced data analytics, and improved revenue. Change Healthcare, the provider of the acquired solution, is recognized for its healthcare claims management software.
Major companies operating in the claims processing software market include Duck Creek Technologies, FINEOS, Hyland Software Inc., Hawksoft Inc., HIPPAsuite, Newgen Software Technologies Limited, Pegasystems Inc., Quick Silver Systems Inc., Ventiv Technology, A1 Enterprise Inc., Applied Systems, Jenesis Software, EIS Group Software, EZLynx, Guidewire Software, ClaimLogiq, Vee Technologies, TriZetto Provider Solutions, Mphasis Limited, Casentric LLC, MedeAnalytics, MedLinks, TriWest Healthcare Alliance, HCL Technologies, HealthEdge Software Inc., Cognizant, McKesson Corporation, HealthTrio LLC, BriteCore, InstaMed, Change Healthcare, Tech Mahindra, eCatalyst Healthcare Solutions, Virtusa, The SSI Group LLC, ClaimVantage, Riskonnect Inc., ReSource Pro, NTT Data, Baker Tilly, EXL Service, Tritech Financial Systems.
North America was the largest region in the claims processing software market in 2024. The regions covered in the claims processing software market report are Asia-Pacific, Western Europe, Eastern Europe, North America, South America, Middle East, Africa. The countries covered in the claims processing software market report are Australia, Brazil, China, France, Germany, India, Indonesia, Japan, Russia, South Korea, UK, USA, Canada, Italy, Spain.
Claims processing software encompasses a software solution designed to execute several critical tasks. This includes risk analysis to assess claim complexity and litigation potential, data analysis to detect fraudulent claims, establishment of automated procedures for claim submissions, and facilitation of support throughout the claims and settlement process.
The primary components of claims processing software consist of software and services. Software refers to a comprehensive set of instructions, data, or computer programs utilized to operate systems and perform specific functions. This software is utilized across various scales of enterprises, including large corporations and small to medium-sized entities such as insurance companies, insurance intermediaries, agents, brokers, and other related entities within the insurance domain.
The claims processing software market research report is one of a series of new reports that provides claims processing software market statistics, including claims processing software industry global market size, regional shares, competitors with a claims processing software market share, detailed claims processing software market segments, market trends, and opportunities, and any further data you may need to thrive in the claims processing software industry. This claims processing software market research report delivers a complete perspective of everything you need, with an in-depth analysis of the current and future scenario of the industry.
The claims processing software market includes revenues earned by entities by providing managing and reviewing insurance claims, data collection, settlement for insurance businesses, payment tracking, recovery tracks, legal matter processing, monitoring, and authorization and authorization processes. The market value includes the value of related goods sold by the service provider or included within the service offering. Only goods and services traded between entities or sold to end consumers are included.
The market value is defined as the revenues that enterprises gain from the sale of goods and/or services within the specified market and geography through sales, grants, or donations in terms of the currency (in USD, unless otherwise specified).
The revenues for a specified geography are consumption values that are revenues generated by organizations in the specified geography within the market, irrespective of where they are produced. It does not include revenues from resales along the supply chain, either further along the supply chain or as part of other products.
This product will be delivered within 3-5 business days.
Table of Contents
Executive Summary
Claims Processing Software Global Market Report 2025 provides strategists, marketers and senior management with the critical information they need to assess the market.This report focuses on claims processing software market which is experiencing strong growth. The report gives a guide to the trends which will be shaping the market over the next ten years and beyond.
Reasons to Purchase:
- Gain a truly global perspective with the most comprehensive report available on this market covering 15 geographies.
- Assess the impact of key macro factors such as conflict, pandemic and recovery, inflation and interest rate environment and the 2nd Trump presidency.
- Create regional and country strategies on the basis of local data and analysis.
- Identify growth segments for investment.
- Outperform competitors using forecast data and the drivers and trends shaping the market.
- Understand customers based on the latest market shares.
- Benchmark performance against key competitors.
- Suitable for supporting your internal and external presentations with reliable high quality data and analysis
- Report will be updated with the latest data and delivered to you along with an Excel data sheet for easy data extraction and analysis.
- All data from the report will also be delivered in an excel dashboard format.
Description
Where is the largest and fastest growing market for claims processing software ? How does the market relate to the overall economy, demography and other similar markets? What forces will shape the market going forward? The claims processing software market global report answers all these questions and many more.The report covers market characteristics, size and growth, segmentation, regional and country breakdowns, competitive landscape, market shares, trends and strategies for this market. It traces the market’s historic and forecast market growth by geography.
- the market characteristics section of the report defines and explains the market.
- the market size section gives the market size ($b) covering both the historic growth of the market, and forecasting its development.
- the forecasts are made after considering the major factors currently impacting the market. These include:
- the forecasts are made after considering the major factors currently impacting the market. These include the Russia-Ukraine war, rising inflation, higher interest rates, and the legacy of the COVID-19 pandemic.
- Market segmentations break down the market into sub markets.
- the regional and country breakdowns section gives an analysis of the market in each geography and the size of the market by geography and compares their historic and forecast growth. It covers the growth trajectory of COVID-19 for all regions, key developed countries and major emerging markets.
- the competitive landscape chapter gives a description of the competitive nature of the market, market shares, and a description of the leading companies. Key financial deals which have shaped the market in recent years are identified.
- the trends and strategies section analyses the shape of the market as it emerges from the crisis and suggests how companies can grow as the market recovers.
Scope
Markets Covered:
1) by Component: Software; Services2) by Enterprise Size: Large Enterprises; Small and Medium-Sized Enterprises
3) by End User: Insurance Companies; Insurance Intermediaries; Agents and Brokers; Other End Users
Subsegments:
1) by Software: Claims Management Software; Billing Software; Policy Administration Software; Reporting and Analytics Software2) by Services: Implementation Services; Maintenance and Support Services; Consulting Services; Training Services
Key Companies Mentioned: Duck Creek Technologies; FINEOS; Hyland Software Inc.; Hawksoft Inc.; HIPPAsuite
Countries: Australia; Brazil; China; France; Germany; India; Indonesia; Japan; Russia; South Korea; UK; USA; Canada; Italy; Spain
Regions: Asia-Pacific; Western Europe; Eastern Europe; North America; South America; Middle East; Africa
Time Series: Five years historic and ten years forecast.
Data: Ratios of market size and growth to related markets, GDP proportions, expenditure per capita.
Data Segmentation: Country and regional historic and forecast data, market share of competitors, market segments.
Sourcing and Referencing: Data and analysis throughout the report is sourced using end notes.
Delivery Format: PDF, Word and Excel Data Dashboard.
Companies Mentioned
Some of the major companies featured in this Claims Processing Software market report include:- Duck Creek Technologies
- FINEOS
- Hyland Software Inc.
- Hawksoft Inc.
- HIPPAsuite
- Newgen Software Technologies Limited
- Pegasystems Inc.
- Quick Silver Systems Inc.
- Ventiv Technology
- A1 Enterprise Inc.
- Applied Systems
- Jenesis Software
- EIS Group Software
- EZLynx
- Guidewire Software
- ClaimLogiq
- Vee Technologies
- TriZetto Provider Solutions
- Mphasis Limited
- Casentric LLC
- MedeAnalytics
- MedLinks
- TriWest Healthcare Alliance
- HCL Technologies
- HealthEdge Software Inc.
- Cognizant
- McKesson Corporation
- HealthTrio LLC
- BriteCore
- InstaMed
- Change Healthcare
- Tech Mahindra
- eCatalyst Healthcare Solutions
- Virtusa
- The SSI Group LLC
- ClaimVantage
- Riskonnect Inc.
- ReSource Pro
- NTT Data
- Baker Tilly
- EXL Service
- Tritech Financial Systems
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 200 |
| Published | February 2025 |
| Forecast Period | 2025 - 2029 |
| Estimated Market Value ( USD | $ 45.74 Billion |
| Forecasted Market Value ( USD | $ 66.23 Billion |
| Compound Annual Growth Rate | 9.7% |
| Regions Covered | Global |
| No. of Companies Mentioned | 43 |