The likelihood of having type 1 diabetes increased when COVID-19 was discovered. Young pediatric patients and older adult patients with COVID-19 had the highest risk. Patients with type 1 diabetes were more likely to contract the virus and experience potentially catastrophic side effects such as diabetic ketoacidosis. Patients required access to diabetes services and get high-quality clinical care, which includes diabetes screening, education, monitoring of complications, and control. The hormone insulin encourages the liver, muscle, and fat cells to absorb glucose from the blood in order to regulate blood sugar levels. It facilitates the absorption of glucose for cellular energy utilization by cells. When the pancreas is unable to create enough insulin, type 1 diabetes develops. Diabetes is frequently thought of as a condition linked to lifestyle. Because of the growing world population, the disease's prevalence has substantially increased over time. Insulin is necessary for everyone with Type 1 diabetes and 10% to 25% of people with Type 2 diabetes or over 100 million people globally. Despite the fact that insulin has been used to treat diabetes for more than 90 years, more than half of the individuals in New Zealand who require it still do not have access to it or can afford it. Insulin As people with type-1 diabetes cannot produce insulin on their own. They require medications and delivery methods. Those with type-2 diabetes also require insulin, especially if they are having problems managing their condition.
New Zealand Oral Anti-Diabetic Drug Market Trends
Sodium-glucose Cotransport-2 (SGLT-2) inhibitor Segment Occupied the Highest Market Share in New Zealand Oral Anti-Diabetic Drugs Market in 2022
In terms of revenue, the Sodium-glucose Cotransport-2 (SGLT-2) inhibitor segment is anticipated to lead the India Oral Anti-Diabetic Drugs Market and post a CAGR of over 2.8% during the course of the forecast year.A hormone produced in the gut called Sodium-glucose Cotransport-2 (SGLT-2) inhibitor promotes the release of insulin, decreases the secretion of glucagon, prevents gastric emptying, and reduces appetite. SGLT2 plasma levels are low during a fast and quickly rise following a meal. By enzymatic breakdown by dipeptidyl peptidase-4 (DPP-4) and renal clearance, circulating levels of intact SGLT2 rapidly drop. SGLT2 operates on GLP-1 receptors found in peripheral tissue, pancreatic islet cells, and other organs and plays a critical role in glucose regulation. By a number of mechanisms, including increased glucose-dependent insulin secretion, delayed stomach emptying, and decreased postprandial glucagon and food intake, GLP-1-based medicines (GLP1-RA and DPP-4 inhibitors) impact glucose control. Obesity, physical inactivity, hypertension, and hyperlipidemia are all frequently linked to T2DM. Those who have their blood sugar levels improperly managed to risk developing long-term microvascular and macrovascular problems. The quality of life and life expectancy is greatly decreased by these problems. T2DM is a complex disorder that places a heavy strain on the patient, their extended family, and the healthcare system. T2DM is thought to affect 5% of New Zealanders, and by 2040, that number is expected to rise to 7% of the population. Compared to other ethnic groups in New Zealand, Pacific, Mori, and South Asian communities are more likely to have T2DM and experience difficulties from the condition.
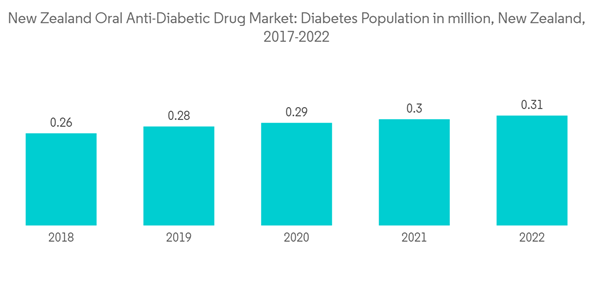
Increasing Diabetes Population in New Zealand is driving the market.
In New Zealand, "primary care" and "secondary care" are widely used to denote different types of medical treatment. The majority of people frequently seek out primary care as their initial form of treatment. This is typically your family physician or general practitioner. Despite the fact that patients must pay for this treatment, those with modest incomes typically qualify for a reduced price. All children under the age of six are eligible to get free doctor visits in New Zealand. Depending on the doctor, GP visits normally cost between NZ 45 and NZ 55. There is no additional cost for a GP visit for foreign travelers. Patients may be directed to secondary care, which is often thought of as specialized treatment, after seeing their physician. Patients may be directed to secondary care, which is often thought of as specialized treatment, after seeing their physician. A few examples of the services that are often managed outside of the major hospitals are hospital services, specialty diabetic services, specialist eye services, specialist renal services, and specialist diabetic services. If a patient is having problems with their diabetes or, in some situations, if they require insulin to treat their diabetes, they can ask to be referred to specialized diabetic services. Some diabetes doctors also run private practices, even though the professional services are free. While the precise cause of type-2 diabetes is unknown, type-1 diabetes is thought to have an unknown origin. The prevalent rate of type-2 diabetes doubled in the last ten years ago. Type 1 diabetes mellitus (T1DM) has increased significantly during the past 20 years. The biggest risk factor for T1DM and the cause of this increase in frequency is the growth in obesity. One of the chronic conditions with the quickest rate of rise in New Zealand is diabetes. Many investigations and surveys have revealed a substantial increase in the population of diabetes, which can be attributed to lifestyle choices.New Zealand Oral Anti-Diabetic Drug Industry Overview
New Zealand's oral anti-diabetes drug market is consolidated, with a few major manufacturers like Eli Lilly, AstraZeneca, Sanofi, and Janssen Pharmaceuticals having a global market presence. While the remaining manufacturers are confined to the other local or regional markets. Companies are focusing on innovations in diabetes drugs.Additional Benefits:
- The market estimate (ME) sheet in Excel format
- 3 months of analyst support
This product will be delivered within 2 business days.
Table of Contents
Companies Mentioned (Partial List)
A selection of companies mentioned in this report includes, but is not limited to:
- Takeda
- Novo Nordisk
- Pfizer
- Eli Lilly
- Janssen Pharmaceuticals
- Astellas
- Boehringer Ingelheim
- Merck And Co.
- AstraZeneca
- Bristol Myers Squibb
- Novartis
- Sanofi