Life insurance providers rely on advanced claims management systems to streamline claim adjudication, reduce manual errors, and improve transparency. The need for robust fraud detection mechanisms also plays a critical role in driving the adoption of these systems as insurers seek to identify and mitigate fraudulent claims. Additionally, the demand for faster settlements and enhanced customer satisfaction has propelled AI-driven claims platforms, enabling insurers to process claims efficiently while maintaining compliance with regulatory standards. Thus, the life insurance claims segment recorded 36% revenue share in the market in 2023.
The integration of predictive analytics in claims management solutions is revolutionizing the insurance and healthcare industries by enabling data-driven decision-making and improving operational efficiency. Predictive analytics utilizes both historical and real-time data to forecast trends, identify potential hazards, and enhance claims processing methodologies. Additionally, automation is a key component of digitized claims management, with technologies like robotic process automation (RPA) and artificial intelligence (AI) driving efficiency. Insurers like Liberty Mutual Insurance use AI-powered chatbots to guide customers through the claims process, collect necessary data, and minimize errors. Therefore, these factors are supporting the growth of the market.
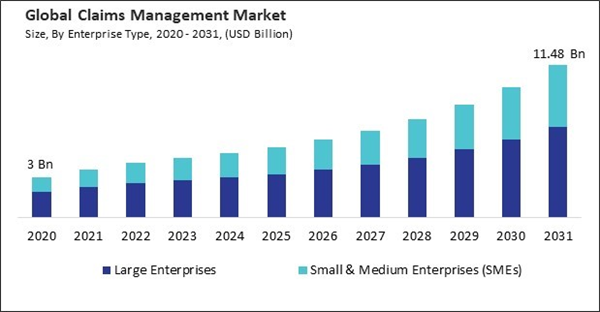
However, Implementing advanced claims management systems can require significant financial investment, particularly for small and medium-sized enterprises (SMEs). These costs often create a substantial barrier for businesses with limited budgets. The initial expenses are not confined to purchasing the software; they extend to critical aspects like system customization, integration with existing IT infrastructure, and user training. Hence, this cost barrier slows the adoption of modern claims management systems.
Driving and Restraining Factors
Drivers- Continuous Rise in Healthcare Costs
- Increasing Use of Analytics
- Rapid Shift Toward Digitization
- Substantially High Implementation Costs
- Data Privacy and Security Concerns
- Integration of Cutting-edge Technologies
- Growing Insurance Penetration
- Complexity of Integrating with Existing IT Infrastructure
- Rising Frequency and Sophistication of Cyberattacks
Enterprise Type Outlook
Based on enterprise type, the market is bifurcated into large enterprises and small & medium enterprises (SMEs). The large enterprises segment garnered 63% revenue share in the market in 2023. These organizations often process high volumes of claims across multiple regions, necessitating systems with capabilities like automation, artificial intelligence, and real-time analytics to ensure accuracy and efficiency.Deployment Outlook
On the basis of deployment mode, the market is classified into cloud and on-premise. The on-premise segment recorded 39% revenue share in the market in 2023. Organizations prioritizing data security and control over their infrastructure drive the segment's growth. Large enterprises, in particular, exhibit a preference for on-premise solutions for the management of sensitive data, including financial and healthcare documents, due to the comprehensive ownership and control they provide. Industries with strict regulatory requirements often opt for on-premise deployment to ensure compliance and mitigate cybersecurity risks.Technology Outlook
By technology, the market is divided into Internet of Things (IoT), Blockchain, robotic process automation (RPA), AI & ML, and others. The robotic process automation (RPA) segment garnered 21% revenue share in the market in 2023. RPA solutions are particularly effective in streamlining data entry, document verification, and claims adjudication processes.End User Outlook
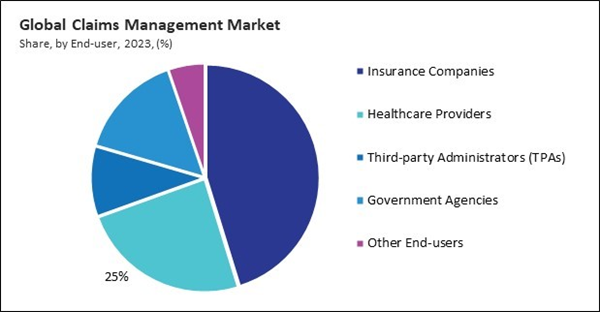
Based on end-user, the market is segmented into insurance companies, healthcare providers, third-party administrators (TPAs), government agencies, and others. The insurance companies segment procured 45% revenue share in the market in 2023. The segment is growing due to its direct involvement in managing many claims across diverse health, life, auto, and property insurance sectors.Type Outlook
On the basis of type, the market is divided into life insurance claims, property & casualty insurance claims, health insurance claims, worker’s compensation claims, disability insurance claims, and others. The property & casualty insurance claims segment garnered 15% revenue share in the market in 2023. Insurers in this segment increasingly rely on IoT technology, such as smart home sensors and telematics, to gather real-time data and assess claims accurately.Regional Outlook
Region-wise, the market is analyzed across North America, Europe, Asia Pacific, and LAMEA. The Europe segment acquired 30% revenue share in the market in 2023. Regulations such as the General Data Protection Regulation (GDPR) have compelled insurers and healthcare providers to implement advanced claims management systems prioritizing secure data handling and transparency.List of Key Companies Profiled
- Salesforce, Inc.
- Conduent, Inc.
- Aclaimant, Inc.
- UnitedHealth Group, Inc. (Optum, Inc.)
- Accenture PLC
- IBM Corporation
- PLEXIS Healthcare Systems, Inc.
- Oracle Corporation
- McKesson Corporation
- DXC Technology Company
Market Report Segmentation
By Enterprise Type- Large Enterprises
- Small & Medium Enterprises (SMEs)
- Cloud
- On-premise
- Internet of Things (IoT)
- Blockchain
- Robotic Process Automation (RPA)
- AI & ML & Other Technologies
- Insurance Companies
- Healthcare Providers
- Third-party Administrators (TPAs)
- Government Agencies
- Other End-users
- Life Insurance Claims
- Property & Casualty Insurance Claims
- Health Insurance Claims
- Worker’s Compensation Claims
- Disability Insurance Claims
- Other Types
- North America
- US
- Canada
- Mexico
- Rest of North America
- Europe
- Germany
- UK
- France
- Russia
- Spain
- Italy
- Rest of Europe
- Asia Pacific
- China
- Japan
- India
- South Korea
- Singapore
- Malaysia
- Rest of Asia Pacific
- LAMEA
- Brazil
- Argentina
- UAE
- Saudi Arabia
- South Africa
- Nigeria
- Rest of LAMEA
Table of Contents
Companies Mentioned
- Salesforce, Inc.
- Conduent, Inc.
- Aclaimant, Inc.
- UnitedHealth Group, Inc. (Optum, Inc.)
- Accenture PLC
- IBM Corporation
- PLEXIS Healthcare Systems, Inc.
- Oracle Corporation
- McKesson Corporation
- DXC Technology Company