Global Healthcare Reimbursement Market - Key Trends & Drivers Summarized
Why Is Healthcare Reimbursement Central to Modern Healthcare Systems?
Healthcare reimbursement is a cornerstone of healthcare financing, ensuring that healthcare providers receive compensation for the services they deliver. This system enables hospitals, clinics, and individual practitioners to maintain financial stability while focusing on delivering quality patient care. As healthcare costs continue to rise globally, efficient reimbursement mechanisms have become crucial for balancing financial sustainability with accessibility. One of the primary factors driving the demand for healthcare reimbursement solutions is the increasing complexity of payment systems. With a growing number of public and private payers, varying coverage plans, and diverse reimbursement models, managing claims and payments has become a challenge for healthcare providers. Advanced reimbursement systems are addressing these challenges by streamlining processes, reducing errors, and accelerating payment cycles. The global shift toward value-based care is another significant trend influencing the healthcare reimbursement market. Unlike traditional fee-for-service models, value-based care emphasizes patient outcomes and cost efficiency. This transition has created a need for reimbursement frameworks that align with performance metrics, such as patient satisfaction, readmission rates, and preventive care outcomes. Reimbursement systems are evolving to support this paradigm, offering tools for tracking and reporting key performance indicators (KPIs).How Is Technology Transforming the Healthcare Reimbursement Landscape?
The integration of technology into healthcare reimbursement processes is revolutionizing how claims are managed and payments are processed. Artificial intelligence (AI) and machine learning (ML) are enabling predictive analytics to identify claim denial trends, optimize coding practices, and detect potential fraud. These technologies not only improve accuracy but also reduce the administrative burden on healthcare providers. Blockchain is emerging as a transformative technology in the reimbursement space, offering secure, transparent, and tamper-proof records of transactions. This innovation is particularly valuable for addressing disputes and ensuring accountability in claims processing. Blockchain-based systems are also facilitating seamless data sharing among payers, providers, and patients, enhancing collaboration and trust across the ecosystem. Cloud-based reimbursement platforms are gaining traction for their scalability and real-time accessibility. These solutions allow providers to manage claims from anywhere, ensuring continuity and adaptability in dynamic healthcare environments. Additionally, robotic process automation (RPA) is automating repetitive tasks such as data entry and claims verification, freeing up resources for strategic financial planning. Together, these technological advancements are driving efficiency, accuracy, and transparency in the healthcare reimbursement process.What Is Driving Demand Across Key Healthcare Segments?
The adoption of healthcare reimbursement systems varies across healthcare settings, with hospitals, outpatient clinics, and specialty care providers being the primary beneficiaries. Hospitals, which manage a high volume of claims and diverse payer contracts, rely heavily on reimbursement solutions to ensure operational efficiency and financial stability. These systems enable hospitals to track claims in real-time, reduce delays, and address denials effectively. Outpatient clinics and specialty care providers are increasingly adopting reimbursement systems to navigate complex billing and coding requirements. The rise of telehealth and home healthcare services has further expanded the need for reimbursement frameworks that cater to non-traditional care settings. Reimbursement solutions tailored for these segments ensure timely payments, enhance patient satisfaction, and support the scalability of remote care delivery models. Regional dynamics also influence market growth, with North America leading the adoption of healthcare reimbursement solutions. The region’ s advanced healthcare infrastructure and regulatory environment drive demand for innovative reimbursement frameworks. In contrast, emerging economies in Asia-Pacific are witnessing rapid growth due to healthcare digitization initiatives, expanding insurance coverage, and the rising prevalence of chronic diseases. These trends highlight the critical role of reimbursement systems in ensuring financial sustainability across diverse healthcare landscapes.What Drives Growth in the Healthcare Reimbursement Market?
The growth in the Healthcare Reimbursement market is driven by several factors, including the increasing complexity of healthcare billing systems and the rising demand for value-based care models. As reimbursement processes become more intricate, advanced systems equipped with AI and automation tools are essential for reducing errors and accelerating payment cycles. The proliferation of telehealth services and home-based care models has also heightened the need for reimbursement frameworks that cater to virtual and decentralized healthcare delivery. Technological advancements, such as blockchain and cloud computing, are significant growth drivers, enabling secure, transparent, and real-time management of claims. Consumer behavior is another critical factor, with patients expecting greater transparency in billing and quicker resolution of claims. Reimbursement systems that offer user-friendly patient portals and mobile apps are gaining popularity for enhancing patient satisfaction and trust. Additionally, regulatory mandates and the push for healthcare digitization are propelling market growth. Governments and private payers are increasingly focusing on fraud prevention, compliance, and cost containment, driving the adoption of sophisticated reimbursement platforms. The expanding coverage of health insurance, particularly in developing regions, is further boosting the demand for reimbursement systems that ensure seamless coordination between payers and providers. These combined factors underscore the essential role of healthcare reimbursement in shaping the future of healthcare financing.Report Scope
The report analyzes the Healthcare Reimbursement market, presented in terms of market value. The analysis covers the key segments and geographic regions outlined below.- Segments: Claim Type (Underpaid Claims, Full Paid Claims); Payer Type (Private Payers, Public Payers); Service Provider (Hospitals Service Provider, Physician's Office Service Provider, Diagnostic Laboratories Service Provider, Other Service Providers).
- Geographic Regions/Countries: World; United States; Canada; Japan; China; Europe (France; Germany; Italy; United Kingdom; Spain; Russia; and Rest of Europe); Asia-Pacific (Australia; India; South Korea; and Rest of Asia-Pacific); Latin America (Argentina; Brazil; Mexico; and Rest of Latin America); Middle East (Iran; Israel; Saudi Arabia; United Arab Emirates; and Rest of Middle East); and Africa.
Key Insights:
- Market Growth: Understand the significant growth trajectory of the Underpaid Claims segment, which is expected to reach US$53.1 Billion by 2030 with a CAGR of a 17.1%. The Full Paid Claims segment is also set to grow at 19.5% CAGR over the analysis period.
- Regional Analysis: Gain insights into the U.S. market, valued at $6.9 Billion in 2024, and China, forecasted to grow at an impressive 23% CAGR to reach $14.8 Billion by 2030. Discover growth trends in other key regions, including Japan, Canada, Germany, and the Asia-Pacific.
Why You Should Buy This Report:
- Detailed Market Analysis: Access a thorough analysis of the Global Healthcare Reimbursement Market, covering all major geographic regions and market segments.
- Competitive Insights: Get an overview of the competitive landscape, including the market presence of major players across different geographies.
- Future Trends and Drivers: Understand the key trends and drivers shaping the future of the Global Healthcare Reimbursement Market.
- Actionable Insights: Benefit from actionable insights that can help you identify new revenue opportunities and make strategic business decisions.
Key Questions Answered:
- How is the Global Healthcare Reimbursement Market expected to evolve by 2030?
- What are the main drivers and restraints affecting the market?
- Which market segments will grow the most over the forecast period?
- How will market shares for different regions and segments change by 2030?
- Who are the leading players in the market, and what are their prospects?
Report Features:
- Comprehensive Market Data: Independent analysis of annual sales and market forecasts in US$ Million from 2024 to 2030.
- In-Depth Regional Analysis: Detailed insights into key markets, including the U.S., China, Japan, Canada, Europe, Asia-Pacific, Latin America, Middle East, and Africa.
- Company Profiles: Coverage of players such as Anaqua, Baker McKenzie, Black Hills IP, Bristows LLP, Cardinal IP and more.
- Complimentary Updates: Receive free report updates for one year to keep you informed of the latest market developments.
Some of the 48 companies featured in this Healthcare Reimbursement market report include:
- Allianz Care
- Aviva plc
- Bajaj Allianz General Insurance Company
- Cigna Healthcare
- CRA International, Inc (Charles River Associates)
- CVS Health Corporation
- OSP LABS
- Reliance Life Insurance
- United HealthCare Services, Inc.
- WellCare Health Plans
This edition integrates the latest global trade and economic shifts into comprehensive market analysis. Key updates include:
- Tariff and Trade Impact: Insights into global tariff negotiations across 180+ countries, with analysis of supply chain turbulence, sourcing disruptions, and geographic realignment. Special focus on 2025 as a pivotal year for trade tensions, including updated perspectives on the Trump-era tariffs.
- Adjusted Forecasts and Analytics: Revised global and regional market forecasts through 2030, incorporating tariff effects, economic uncertainty, and structural changes in globalization. Includes historical analysis from 2015 to 2023.
- Strategic Market Dynamics: Evaluation of revised market prospects, regional outlooks, and key economic indicators such as population and urbanization trends.
- Innovation & Technology Trends: Latest developments in product and process innovation, emerging technologies, and key industry drivers shaping the competitive landscape.
- Competitive Intelligence: Updated global market share estimates for 2025, competitive positioning of major players (Strong/Active/Niche/Trivial), and refined focus on leading global brands and core players.
- Expert Insight & Commentary: Strategic analysis from economists, trade experts, and domain specialists to contextualize market shifts and identify emerging opportunities.
Table of Contents
Companies Mentioned (Partial List)
A selection of companies mentioned in this report includes, but is not limited to:
- Allianz Care
- Aviva plc
- Bajaj Allianz General Insurance Company
- Cigna Healthcare
- CRA International, Inc (Charles River Associates)
- CVS Health Corporation
- OSP LABS
- Reliance Life Insurance
- United HealthCare Services, Inc.
- WellCare Health Plans
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 378 |
| Published | February 2026 |
| Forecast Period | 2024 - 2030 |
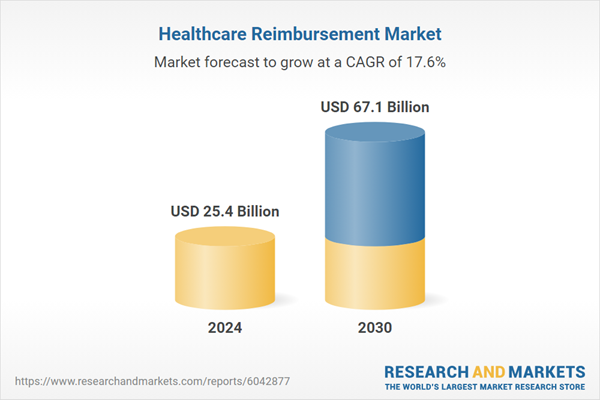
| Estimated Market Value ( USD | $ 25.4 Billion |
| Forecasted Market Value ( USD | $ 67.1 Billion |
| Compound Annual Growth Rate | 17.6% |
| Regions Covered | Global |