Chapter 1 Methodology and Scope
1.1 Market Segmentation & Scope
1.1.1 Segment Definition
1.1.1.1 Solution coverage
1.1.1.2 Buyer type
1.1.1.3 Value chain processes
1.1.1.4 Buyer size
1.2 Research Methodology
1.2.1 Information procurement
1.2.1.1 Purchased database
1.2.1.2 Internal database
1.2.1.3 Secondary sources
1.2.1.4 Primary research
1.3 Information or Data Analysis
1.3.1 Data Analysis Models
1.4 Market Formulation & Validation
1.5 Model Details
1.6 List of Secondary Sources
1.7 List of Abbreviations
1.8 Objectives
1.8.1 Objective - 1
1.8.2 Objective - 2
1.8.3 Objective - 3
Chapter 2 Executive Summary
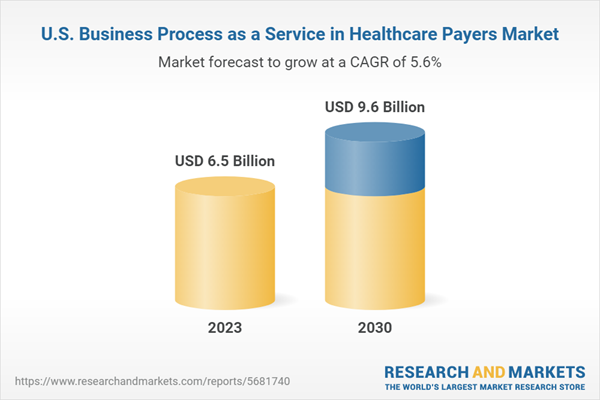
2.1 Market Outlook
2.2 Segment Snapshot
2.3 Competitive Landscape
Chapter 3 Market Variables, Trends & Scope
3.1 Market Lineage Outlook
3.1.1 Parent Market Outlook
3.1.2 Related/Ancillary Market Outlook
3.2 Market Dynamics
3.2.1 Market Driver Analysis
3.2.1.1 Changing regulations
3.2.1.2 Expanding healthcare consumerism
3.2.1.3 Shift towards value-based healthcare
3.2.2 Market Restraint Analysis
3.2.2.1 Risk Concerns Regarding Data Security
3.2.2.2 High costs
3.3 Business Environment Analysis Tools
3.3.1 Porter’s Five Forces Analysis
3.3.2 PESTLE Analysis
3.4 Impact of COVID-19 on U.S. Business Process as a Service (BPaaS) in Healthcare Payer Market
3.5 Regulatory Framework
Chapter 4 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market: Solution Coverage Estimates & Trend Analysis
4.1 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market Solution Coverage Type Movement Analysis, 2023 & 2030
4.2 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market: Solution Coverage Segment Dashboard
4.3 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market Size & Forecast and Forecasts, By Solution Coverage (USD Billion)
4.3.1 Traditional BPaaS
4.3.1.1 Traditional BPaaS market, 2018 - 2030 (USD Billion)
4.3.1.2 End-to-end traditional BPaaS
4.3.1.2.1 End-to-end traditional BPaaS market, 2018 - 2030 (USD Billion)
4.3.1.3 Process-specific traditional BPaaS
4.3.1.3.1 Process-specific traditional BPaaS market, 2018 - 2030 (USD Billion)
4.3.2 Best-of-Breed bpaas
4.3.2.1 Best-of-breed bpaas market, 2018 - 2030 (USD Billion)
4.3.2.2 End-to-end best-of-breed BPaaS
4.3.2.2.1 End-to-end best-of-breed BPaaS market, 2018 - 2030 (USD Billion)
4.3.2.3 Process-specific best-of-breed BPaaS
4.3.2.3.1 Process-specific best-of-breed BPaaS market, 2018 - 2030 (USD Billion)
Chapter 5 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market: Buyer Type Estimates & Trend Analysis
5.1 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market Buyer Type Movement Analysis, 2023 & 2030
5.2 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market: Buyer Type Segment Dashboard
5.3 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market Size & Forecast and Forecasts, By Buyer Type (USD Billion)
5.3.1 Government buyers
5.3.1.1 Government Buyers Market, 2018 - 2030 (USD Billion)
5.3.1.2 Medicare advantage
5.3.1.2.1 Medicare Advantage Market, 2018 - 2030 (USD Billion)
5.3.1.3 Managed Medicaid
5.3.1.3.1 Managed Medicaid market, 2018 - 2030 (USD Billion)
5.3.2 Commerical buyers
5.3.2.1 Commercial Buyers Market, 2018 - 2030 (USD Billion)
5.3.2.2 Individual Health Plans
5.3.2.2.1 Individual health plans market, 2018 - 2030 (USD Billion)
5.3.2.3 Employer-sponsored health plan
5.3.2.3.1 Employer sponsored health plan market, 2018 - 2030 (USD Billion)
Chapter 6 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market: Value Chain Processes Estimates & Trend Analysis
6.1 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market Value Chain Processes Movement Analysis, 2023 & 2030
6.2 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market: Value Chain Processes Segment Dashboard
6.3 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market Size & Forecast and Forecasts, By Value Chain Processes (USD Billion)
6.3.1 Claims Management
6.3.1.1 Claims Management Market, 2018 - 2030 (USD Billion)
6.3.2 Member engagement
6.3.2.1 Member engagement market, 2018 - 2030 (USD Billion)
6.3.3 Care management
6.3.3.1 Care management market, 2018 - 2030 (USD Billion)
6.3.4 Others
6.3.4.1 Others market, 2018 - 2030 (USD Billion)
Chapter 7 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market: Buyer Size Estimates & Trend Analysis
7.1 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market Buyer Size Movement Analysis, 2023 & 2030
7.2 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market: Buyer Size Segment Dashboard
7.3 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market Size & Forecast and Forecasts, By Buyer Size (USD Billion)
7.3.1 Small buyers
7.3.1.1 Small Buyers Market, 2018 - 2030 (USD Billion)
7.3.2 Mid-sized buyers
7.3.2.1 Mid-sized buyers market, 2018 - 2030 (USD Billion)
7.3.3 Large buyers
7.3.3.1 Large Buyers Market, 2018 - 2030 (USD Billion)
Chapter 8 Competitive Analysis
8.1 Participant Categorization
8.2 Company Market Position Analysis
8.3 Strategy Mapping
8.3.1 New Launch
8.3.2 Mergers & acquisition
8.3.3 Partnerships
8.3.4 Collaborations
8.5.5 Others
8.4 Company Profiles/ Listing
8.4.1 Accenture
8.4.1.1 Company overview
8.4.1.2 Financial performance
8.4.1.3 Product benchmarking
8.4.1.4 Strategic initiatives
8.4.2 Cognizant
8.4.2.1 Company overview
8.4.2.2 Financial performance
8.4.2.3 Product benchmarking
8.4.2.4 Strategic initiatives
8.4.3 HCL Technologies Limited
8.4.3.1 Company overview
8.4.3.2 Financial performance
8.4.3.3 Product benchmarking
8.4.3.4 Strategic initiatives
8.4.4 IBM
8.4.4.1 Company overview
8.4.4.2 Financial performance
8.4.4.3 Product benchmarking
8.4.4.4 Strategic initiatives
8.4.5 Infosys Limited
8.4.5.1 Company overview
8.4.5.2 Financial performance
8.4.5.3 Product benchmarking
8.4.5.4 Strategic initiatives
8.4.6 NTT DATA Corporation
8.4.6.1 Company overview
8.4.6.2 Financial performance
8.4.6.3 Product benchmarking
8.4.6.4 Strategic initiatives
8.4.7 Optum
8.4.7.1 Company overview
8.4.7.2 Financial performance
8.4.7.3 Product benchmarking
8.4.7.4 Strategic initiatives
8.4.8 TATA Consultancy Services Limited
8.4.8.1 Company overview
8.4.8.2 Financial performance
8.4.8.3 Product benchmarking
8.4.8.4 Strategic initiatives
8.4.9 UST
8.4.9.1 Company overview
8.4.9.2 Financial performance
8.4.9.3 Product benchmarking
8.4.9.4 Strategic initiatives
8.4.10 Wipro
8.4.10.1 Company overview
8.4.10.2 Financial performance
8.4.10.3 Product benchmarking
8.4.10.4 Strategic initiatives
8.4.11 EXL
8.4.11.1 Company overview
8.4.11.2 Financial performance
8.4.11.3 Product benchmarking
8.4.11.4 Strategic initiatives
8.4.12 Softheon, Inc.
8.4.12.1 Company overview
8.4.12.2 Financial performance
8.4.12.3 Product benchmarking
8.4.12.4 Strategic initiatives
8.4.13 Genpact
8.4.13.1 Company overview
8.4.13.2 Financial performance
8.4.13.3 Product benchmarking
8.4.13.4 Strategic initiatives
8.4.14 Change Healthcare
8.4.14.1 Company overview
8.4.14.2 Financial performance
8.4.14.3 Product benchmarking
8.4.14.4 Strategic initiatives
8.4.15 Firstsource
8.4.15.1 Company overview
8.4.15.2 Financial performance
8.4.15.3 Product benchmarking
8.4.15.4 Strategic initiatives
8.4.16 Celegence
8.4.16.1 Company overview
8.4.16.2 Financial performance
8.4.16.3 Product benchmarking
8.4.16.4 Strategic initiatives
8.4.17 Highmark Health
8.4.17.1 Company overview
8.4.17.2 Financial performance
8.4.17.3 Product benchmarking
8.4.17.4 Strategic initiatives
List of Tables
Table 1 List of secondary sources
Table 2 List of key companies
Table 3 U.S. Business Process as a Service (BPaaS) in healthcare payers market, by solution coverage, 2018 - 2030 (USD Billion)
Table 4 U.S. Business Process as a Service (BPaaS) in healthcare payers market, by traditional BPaaS, 2018 - 2030 (USD Billion)
Table 5 U.S. Business Process as a Service (BPaaS) in healthcare payers market, best-of-breed BPaaS, 2018 - 2030 (USD Billion)
Table 6 U.S. Business Process as a Service (BPaaS) in healthcare payers market, by buyer type, 2018 - 2030 (USD Billion)
Table 7 U.S. Business Process as a Service (BPaaS) in healthcare payers market, by commercial buyers, 2018 - 2030 (USD Billion)
Table 8 U.S. Business Process as a Service (BPaaS) in healthcare payers market, by value chain processes, 2018 - 2030 (USD Billion)
Table 9 U.S. Business Process as a Service (BPaaS) in Healthcare Payers Market, By Buyer Size, 2018 - 2030 (USD Billion)
List of Figures
Fig. 1 U.S. business process as a Service in healthcare payers segmentation
Fig. 2 Market research process
Fig. 3 Data triangulation techniques
Fig. 4 Primary research pattern
Fig. 5 Market research approaches
Fig. 6 Value chain-based sizing & forecasting
Fig. 7 QFD modeling for market share assessment
Fig. 8 Market formulation & validation
Fig. 9 Market snapshot
Fig. 10 Segment outlook
Fig. 11 Segment outlook
Fig. 12 Competitive landscape
Fig. 13 U.S. business process as a service in healthcare payers market lineage
Fig. 14 Parent market outlook
Fig. 15 Related market outlook
Fig. 16 U.S. Business process as a service in Healthcare payers market dynamics
Fig. 17 U.S. business process as a service in healthcare payers market: Porter’s analysis
Fig. 18 U.S. business process as a service in healthcare payers market: PESTLE analysis
Fig. 19 U.S. business process as a service in healthcare payers market: Solution coverage movement share analysis, (USD Billion)
Fig. 20 U.S. business process as a service in healthcare payers market: Solution coverage segment dashboard
Fig. 21 Traditional BPaaS market, 2018 - 2030 (USD Billion)
Fig. 22 End-to-end traditional BPaaS market, 2018 - 2030 (USD Billion)
Fig. 23 Process specific traditional BPaaS market, 2018 - 2030 (USD Billion)
Fig. 24 Best-of-breed BPaaS market, 2018 - 2030 (USD Billion)
Fig. 25 End-to-end best-of-breed BPaaS market, 2018 - 2030 (USD Billion)
Fig. 26 Process specific best-of-breed BPaaS market, 2018 - 2030 (USD Billion)
Fig. 27 U.S. business process as a service in healthcare payers market: Buyer type movement share analysis, (USD Billion)
Fig. 28 U.S. business process as a service in healthcare payers market: Buyer type segment dashboard
Fig. 29 Government buyers market, 2018 - 2030 (USD Billion)
Fig. 30 Medicare advantage market, 2018 - 2030 (USD Billion )
Fig. 31 Managed Medicaid market, 2018 - 2030 (USD Billion )
Fig. 32 Commercial buyers market, 2018 - 2030 (USD Billion)
Fig. 33 Individual health plans market, 2018 - 2030 (USD Billion)
Fig. 34 Employer sponsored health plan market, 2018 - 2030 (USD Billion)
Fig. 35 U.S. business process as a service in healthcare payers market: Value chain process movement share analysis, (USD Billion)
Fig. 36 U.S. business process as a service in healthcare payers market: Value chain processes segment dashboard
Fig. 37 Claims management market, 2018 - 2030 (USD Billion)
Fig. 38 Member engagement market, 2018 - 2030 (USD Billion)
Fig. 39 Care management market, 2018 - 2030 (USD Billion)
Fig. 40 Others market, 2018 - 2030 (USD Billion)
Fig. 41 U.S. business process as a service in healthcare payers market: Buyer size movement share analysis, (USD Billion)
Fig. 42 U.S. business process as a service in healthcare payers market: Buyer size segment dashboard
Fig. 43 Small buyers market, 2018 - 2030 (USD Billion)
Fig. 44 Mid-sized buyers market, 2018 - 2030 (USD Billion)
Fig. 45 Large buyers market, 2018 - 2030 (USD Billion)
Fig. 46 Company/competition categorization
Fig. 47 Company market position analysis
Fig. 48 Strategy mapping
Fig. 49 Acquisition mapping