Global Healthcare Claims Management Market - Key Trends and Drivers Summarized
Why Is Healthcare Claims Management Becoming Essential for Streamlining Reimbursement Processes, Reducing Errors, and Enhancing Financial Performance in Healthcare Organizations?
Healthcare claims management has become essential for streamlining reimbursement processes, reducing errors, and enhancing the financial performance of healthcare organizations. But why is claims management so critical today? In an increasingly complex healthcare landscape, where providers must navigate various insurance plans, coding systems, and regulatory requirements, claims management ensures that healthcare facilities are reimbursed accurately and promptly for the services they provide. This process involves submitting, tracking, and processing claims to insurance companies for the care rendered to patients. Efficient claims management helps avoid delays in payments, which can significantly impact a healthcare provider's revenue cycle and overall financial health.Moreover, healthcare claims management reduces administrative burdens by automating many of the manual processes involved in claims submission. It also ensures compliance with the ever-evolving healthcare regulations and payer requirements, helping providers avoid costly penalties or rejections. Claims management systems streamline the process of verifying patient eligibility, coding medical services correctly, and resolving denied claims. This optimization is crucial for healthcare organizations to maintain financial stability and operational efficiency while delivering high-quality care to their patients.
How Are Technological Advancements and Innovations Improving the Accuracy, Speed, and Efficiency of Healthcare Claims Management?
Technological advancements are significantly improving the accuracy, speed, and efficiency of healthcare claims management, making it easier for healthcare organizations to handle complex billing processes. One of the most impactful innovations is the widespread adoption of claims management software that automates key steps in the claims process. These platforms use artificial intelligence (AI) and machine learning (ML) algorithms to review claims for accuracy, ensuring that patient information, medical codes, and insurance details are correct before submission. By automating these checks, healthcare providers can reduce human errors, which are one of the leading causes of claim denials.Another major advancement is the integration of claims management systems with electronic health records (EHRs) and practice management software. This integration allows for seamless data sharing between clinical and billing departments, ensuring that medical codes and patient information are accurate and up-to-date. When claims are submitted with correct details from the start, the chances of claim denials are significantly reduced, speeding up the reimbursement process. Moreover, this integration ensures that healthcare providers can access real-time updates on claim statuses, track reimbursements, and quickly address any issues that arise.
Robotic process automation (RPA) is also revolutionizing healthcare claims management by automating repetitive tasks such as data entry, claims tracking, and patient eligibility verification. RPA tools can process large volumes of claims quickly and accurately, freeing up administrative staff to focus on more complex tasks like resolving denied claims or addressing patient inquiries. This level of automation not only reduces processing time but also helps healthcare organizations handle a higher volume of claims with fewer resources, improving overall operational efficiency.
Blockchain technology is another promising innovation in healthcare claims management. Blockchain's decentralized, tamper-proof ledger system can streamline the claims submission process by providing secure, transparent records that all parties (providers, payers, and patients) can access. This transparency reduces disputes over billing and ensures that all parties have access to the same accurate information. Blockchain also enhances security by protecting sensitive patient and financial data from fraud and unauthorized access, ensuring that healthcare organizations comply with regulatory standards like HIPAA.
The use of predictive analytics and data analytics tools is also improving claims management by helping providers identify patterns that may lead to denials or delays. By analyzing historical claims data, these tools can identify trends such as frequently denied procedures, common coding errors, or payer-specific requirements. This insight allows healthcare providers to adjust their claims submission processes proactively, reducing the likelihood of errors and improving the chances of first-time claim acceptance. Analytics tools can also help predict future cash flow, providing healthcare organizations with a clearer picture of their financial health.
Why Is Healthcare Claims Management Critical for Reducing Denials, Optimizing Revenue Cycles, and Ensuring Regulatory Compliance?
Healthcare claims management is critical for reducing claim denials, optimizing revenue cycles, and ensuring regulatory compliance because it directly impacts the financial health and operational efficiency of healthcare providers. One of the main reasons healthcare claims management is so valuable is its ability to minimize claim denials, which are a leading cause of revenue loss in healthcare organizations. Claims can be denied for a variety of reasons, including incorrect coding, missing patient information, or issues with insurance eligibility. Effective claims management systems use automation and real-time data validation to ensure that claims are submitted accurately the first time, reducing the chances of denial and the costly rework involved in resubmitting claims.Optimizing the revenue cycle is another key benefit of healthcare claims management. The revenue cycle encompasses the entire process of patient care, from scheduling appointments and verifying insurance coverage to providing services and receiving payment from payers. Claims management plays a crucial role in ensuring that this process runs smoothly by reducing delays in reimbursement and increasing the rate of claims acceptance. When claims are processed efficiently, healthcare providers can maintain a steady cash flow, ensuring that they have the financial resources needed to operate effectively and continue delivering high-quality care to their patients.
Ensuring regulatory compliance is another critical function of healthcare claims management. The healthcare industry is subject to numerous regulations, including the Health Insurance Portability and Accountability Act (HIPAA), the Affordable Care Act (ACA), and various payer-specific requirements. Claims management systems help providers stay compliant with these regulations by automating the submission of accurate, complete claims and ensuring that all patient and financial data is securely handled. Failing to comply with regulatory requirements can lead to penalties, audits, and even legal action, all of which can have severe financial and reputational consequences for healthcare organizations. By automating the compliance process, claims management systems help providers mitigate these risks and maintain the highest standards of data security and accuracy.
Effective claims management also improves patient satisfaction by reducing billing errors and disputes. Patients expect transparency and accuracy when it comes to their healthcare costs, and errors in billing or denied claims can lead to frustration and financial stress. By ensuring that claims are processed accurately and in a timely manner, healthcare providers can offer a smoother billing experience for their patients, leading to higher levels of trust and satisfaction. Additionally, automated systems can provide patients with detailed breakdowns of their costs, helping them better understand their financial responsibility and any insurance coverage details.
Moreover, claims management systems offer healthcare organizations valuable insights into their financial performance. Through detailed reporting and analytics, providers can track key metrics such as claim acceptance rates, denial trends, and reimbursement times. This data-driven approach allows healthcare administrators to identify bottlenecks or inefficiencies in their claims processes, making it easier to implement targeted improvements and optimize the overall revenue cycle.
What Factors Are Driving the Growth of the Healthcare Claims Management Market?
Several key factors are driving the rapid growth of the healthcare claims management market, including the increasing complexity of healthcare billing and coding, advancements in automation technologies, the rising demand for cost-effective healthcare solutions, and the push for value-based care models. One of the primary drivers is the growing complexity of healthcare billing and coding systems. As healthcare services become more specialized and payer requirements more varied, providers must navigate an intricate web of codes, rules, and regulations to ensure accurate billing. Claims management solutions offer a streamlined way to manage this complexity by automating coding processes, reducing the risk of errors, and ensuring that claims comply with payer requirements.The advancement of automation technologies such as AI, machine learning, and robotic process automation (RPA) is another significant factor contributing to the growth of the claims management market. These technologies enable healthcare providers to process large volumes of claims quickly and accurately, reducing administrative costs and improving operational efficiency. Automated claims management systems can also handle more complex tasks, such as identifying patterns that lead to denials or predicting future cash flow based on historical claims data. As healthcare organizations look for ways to reduce costs while improving service quality, the adoption of automated claims management solutions is becoming increasingly widespread.
The rising demand for cost-effective healthcare solutions is further fueling the growth of the claims management market. As healthcare costs continue to rise, both providers and patients are seeking ways to reduce expenses without compromising the quality of care. Effective claims management helps providers maintain a healthy revenue cycle by reducing denied claims and ensuring timely reimbursements, allowing them to continue delivering care while keeping operational costs in check. For patients, accurate claims processing reduces the risk of billing errors and unexpected charges, improving the overall experience of receiving healthcare services.
The shift toward value-based care models is another key driver of market growth. Value-based care emphasizes improving patient outcomes while controlling costs, shifting the focus away from the volume of services provided and toward the quality of care delivered. Claims management plays a critical role in this shift by enabling providers to track and report on key performance indicators (KPIs) related to patient outcomes, quality of care, and cost-efficiency. By optimizing claims processes and improving revenue cycle management, healthcare providers can align their operations with value-based care initiatives, improving both financial performance and patient satisfaction.
Additionally, regulatory changes and healthcare reforms, such as the Affordable Care Act (ACA) in the U.S., have placed greater emphasis on accurate claims processing and timely reimbursement. These regulations often require providers to adhere to new standards for coding, billing, and reporting, which has increased the need for sophisticated claims management systems that can ensure compliance. As regulations continue to evolve, healthcare organizations must invest in claims management solutions that can adapt to these changes, further driving the demand for advanced claims management technologies.
In conclusion, the growth of the healthcare claims management market is driven by increasing billing complexity, advancements in automation technologies, the demand for cost-efficient healthcare solutions, and the shift toward value-based care models. As healthcare organizations continue to face challenges in managing the revenue cycle, claims management systems will remain essential tools for optimizing financial performance, ensuring regulatory compliance, and improving overall patient care delivery.
Report Scope
The report analyzes the Healthcare Claims Management market, presented in terms of market value (USD). The analysis covers the key segments and geographic regions outlined below.- Segments: Component (Software, Services); Type (Standalone, Integrated); Deployment (On-Premise, Cloud); End-Use (Healthcare Providers, Healthcare Payers, Other End-Uses).
- Geographic Regions/Countries: World; United States; Canada; Japan; China; Europe (France; Germany; Italy; United Kingdom; and Rest of Europe); Asia-Pacific; Rest of World.
Key Insights:
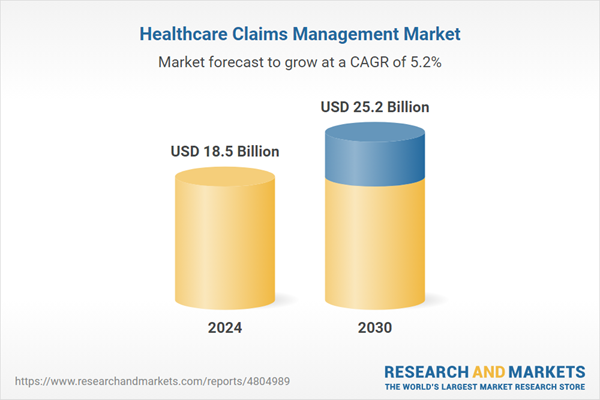
- Market Growth: Understand the significant growth trajectory of the Standalone Claims Management segment, which is expected to reach US$16.1 Billion by 2030 with a CAGR of 4.9%. The Integrated Claims Management segment is also set to grow at 5.9% CAGR over the analysis period.
- Regional Analysis: Gain insights into the U.S. market, valued at $5.1 Billion in 2024, and China, forecasted to grow at an impressive 5% CAGR to reach $4 Billion by 2030. Discover growth trends in other key regions, including Japan, Canada, Germany, and the Asia-Pacific.
Why You Should Buy This Report:
- Detailed Market Analysis: Access a thorough analysis of the Global Healthcare Claims Management Market, covering all major geographic regions and market segments.
- Competitive Insights: Get an overview of the competitive landscape, including the market presence of major players across different geographies.
- Future Trends and Drivers: Understand the key trends and drivers shaping the future of the Global Healthcare Claims Management Market.
- Actionable Insights: Benefit from actionable insights that can help you identify new revenue opportunities and make strategic business decisions.
Key Questions Answered:
- How is the Global Healthcare Claims Management Market expected to evolve by 2030?
- What are the main drivers and restraints affecting the market?
- Which market segments will grow the most over the forecast period?
- How will market shares for different regions and segments change by 2030?
- Who are the leading players in the market, and what are their prospects?
Report Features:
- Comprehensive Market Data: Independent analysis of annual sales and market forecasts in US$ Million from 2024 to 2030.
- In-Depth Regional Analysis: Detailed insights into key markets, including the U.S., China, Japan, Canada, Europe, Asia-Pacific, Latin America, Middle East, and Africa.
- Company Profiles: Coverage of players such as Allscripts Healthcare Solutions, Inc., Athenahealth, Inc., Cerner Corporation, Cognizant Technology Solutions Corporation, Conifer Health Solutions, LLC. and more.
- Complimentary Updates: Receive free report updates for one year to keep you informed of the latest market developments.
Some of the 41 companies featured in this Healthcare Claims Management market report include:
- Allscripts Healthcare Solutions, Inc.
- Athenahealth, Inc.
- Cerner Corporation
- Cognizant Technology Solutions Corporation
- Conifer Health Solutions, LLC.
- Context4 Healthcare Inc.
- DST Systems, Inc.
- eClinicalWorks LLC
- GE Healthcare
- GeBBS Healthcare Solutions, Inc.
- Health Solutions Plus
- McKesson Corporation
- nThrive, Inc.
- Optum, Inc.
- PLEXIS Healthcare Systems, Inc.
- Quest Diagnostics, Inc.
- Ram Technologies, Inc.
- The SSI Group, LLC
This edition integrates the latest global trade and economic shifts into comprehensive market analysis. Key updates include:
- Tariff and Trade Impact: Insights into global tariff negotiations across 180+ countries, with analysis of supply chain turbulence, sourcing disruptions, and geographic realignment. Special focus on 2025 as a pivotal year for trade tensions, including updated perspectives on the Trump-era tariffs.
- Adjusted Forecasts and Analytics: Revised global and regional market forecasts through 2030, incorporating tariff effects, economic uncertainty, and structural changes in globalization. Includes historical analysis from 2015 to 2023.
- Strategic Market Dynamics: Evaluation of revised market prospects, regional outlooks, and key economic indicators such as population and urbanization trends.
- Innovation & Technology Trends: Latest developments in product and process innovation, emerging technologies, and key industry drivers shaping the competitive landscape.
- Competitive Intelligence: Updated global market share estimates for 2025, competitive positioning of major players (Strong/Active/Niche/Trivial), and refined focus on leading global brands and core players.
- Expert Insight & Commentary: Strategic analysis from economists, trade experts, and domain specialists to contextualize market shifts and identify emerging opportunities.
Table of Contents
Companies Mentioned (Partial List)
A selection of companies mentioned in this report includes, but is not limited to:
- Allscripts Healthcare Solutions, Inc.
- Athenahealth, Inc.
- Cerner Corporation
- Cognizant Technology Solutions Corporation
- Conifer Health Solutions, LLC.
- Context4 Healthcare Inc.
- DST Systems, Inc.
- eClinicalWorks LLC
- GE Healthcare
- GeBBS Healthcare Solutions, Inc.
- Health Solutions Plus
- McKesson Corporation
- nThrive, Inc.
- Optum, Inc.
- PLEXIS Healthcare Systems, Inc.
- Quest Diagnostics, Inc.
- Ram Technologies, Inc.
- The SSI Group, LLC
Table Information
| Report Attribute | Details |
|---|---|
| No. of Pages | 194 |
| Published | February 2026 |
| Forecast Period | 2024 - 2030 |
| Estimated Market Value ( USD | $ 18.5 Billion |
| Forecasted Market Value ( USD | $ 25.1 Billion |
| Compound Annual Growth Rate | 5.2% |
| Regions Covered | Global |